Table of Contents
Introduction: The Untold Story of Male Fertility
As a physician who has spent years studying male reproductive health and treating complex fertility cases, I can say without hesitation that varicocele is one of the most significant yet underestimated conditions in men’s health. It’s a condition that’s easy to recognize, even easier to ignore, but its long-term effects on quality of life, fertility, and hormonal health can be profound.
Think of varicocele like varicose veins in your legs, except these swollen veins are located in your scrotum. Some men live with varicoceles for decades without symptoms, while others face chronic discomfort, testicular shrinkage, or infertility. What’s particularly striking is the difference in prevalence between the general population (15-20%) and men seeking fertility treatment (up to 80%).
This comprehensive guide combines clinical experience, colleague insights, and the latest research from 2024-2025 to provide you with clear, authoritative information about varicocele. My goal isn’t just to inform—it’s to equip patients and their partners with deep understanding so they can make informed decisions about management and treatment.
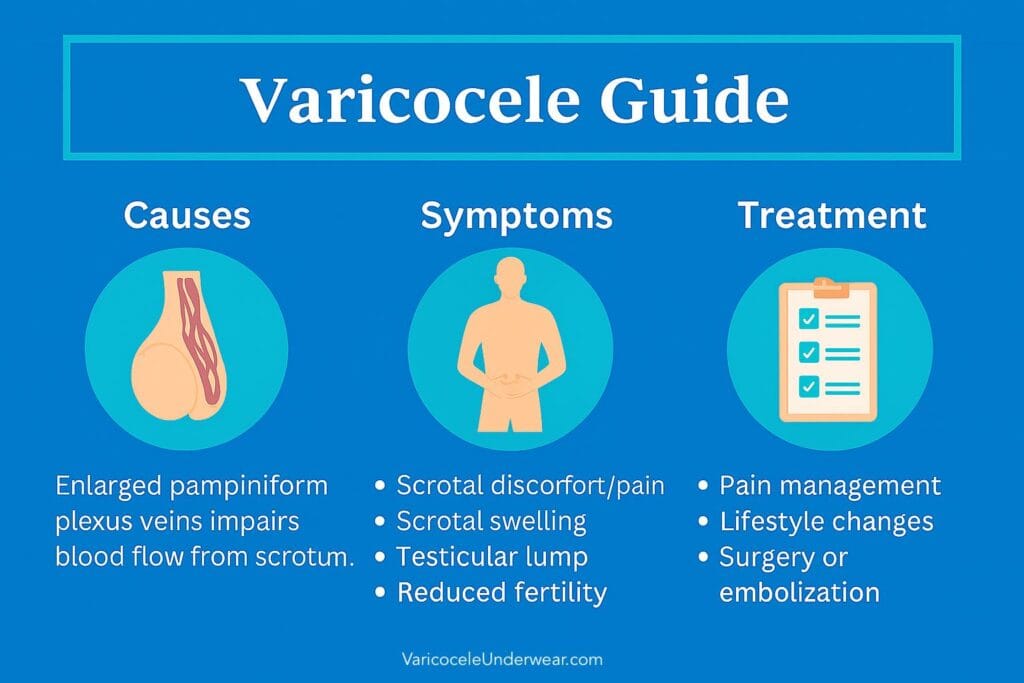
What is Varicocele? More Than Just Swollen Veins
The term comes from the Latin word “varix” (swollen vein) and the Greek word “kele” (swelling). In medical terms, varicocele refers to abnormal enlargement of the pampiniform plexus veins in the scrotum.
This plexus isn’t just a collection of blood vessels—it functions as a sophisticated heat exchanger. Blood coming from your abdomen toward your testicles is warm, while blood returning from your testicles is cooler. This plexus allows heat transfer from arterial blood to venous blood, effectively cooling your testicles before blood enters them. Healthy testicles are about 2-3 degrees Celsius cooler than body temperature, which is crucial for sperm production.
In my patient conversations, I often describe this as a “cooling system problem.” When veins enlarge and fail, this system collapses. Blood begins to pool, heat accumulates, and over time, testicular function declines. This isn’t a static condition—it’s a progressive disorder that can silently cause damage.
How Common are Varicoceles?
Based on the latest 2024-2025 research and clinical data, here’s what we know:
General Population Statistics
- 15-20% of all men have varicoceles
- 10-20% prevalence in healthy males according to recent Korean guidelines
Infertility Connection
The numbers become more striking when we look at men with fertility problems:
- 35-40% of men with primary infertility have varicoceles
- Up to 81% of men with secondary infertility (those who previously had children but now face difficulties) have varicoceles
- Recent studies show 32% overall prevalence among infertile men
These statistics alone tell us about their potential impact on male fertility.
Are Varicoceles Normal, Harmless, or Dangerous?
Common: Yes, they’re extremely common. Every urologist sees them weekly.
Normal: No, they’re not part of normal anatomy. However, they’re so common that they’re “normal” in terms of clinical presentation.
Often Harmless: The majority of men with varicoceles never develop symptoms requiring treatment.
Potentially Harmful: When associated with infertility, testicular atrophy (shrinkage), or chronic pain, varicoceles are anything but harmless. Sperm damage, decreased testosterone levels, and progressive worsening are real risks.
Persistent: In my experience, and consistent with medical literature, they almost never resolve spontaneously. Once developed, they’re usually there to stay.
Symptoms and Self-Examination Guide
Varicoceles are classified into three grades:
Grade Classification System
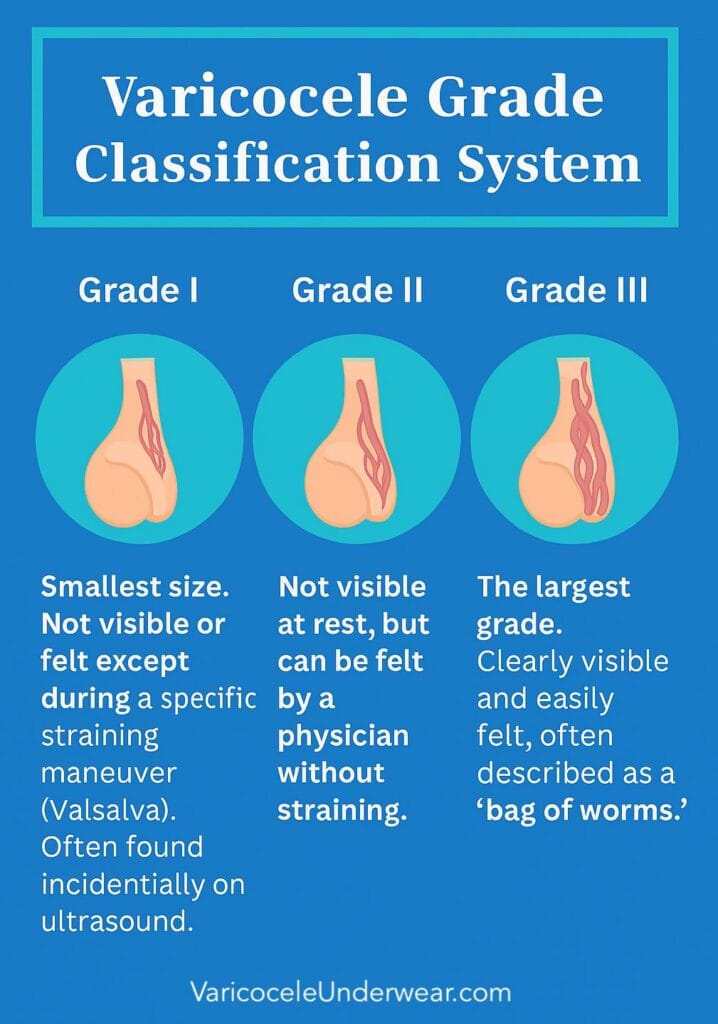
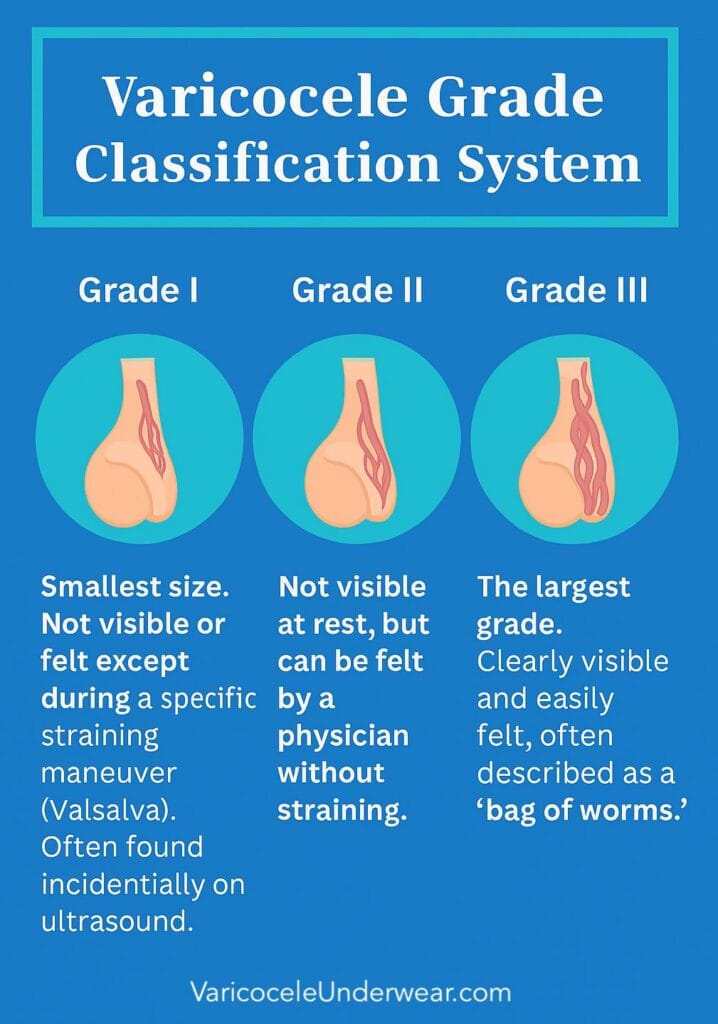
| Grade | Description |
|---|---|
| Grade I | Smallest size. Not visible or felt except during a specific straining maneuver (Valsalva). Often found incidentally on ultrasound. |
| Grade II | Not visible at rest, but can be felt by a physician without straining. |
| Grade III | The largest grade. Clearly visible and easily felt, often described as a “bag of worms.” |
How Varicoceles Look and Feel
Men with symptoms typically describe:
Appearance: Vein clusters that become more visible after physical activity, prolonged standing, or hot showers.
Touch: Soft, worm-like texture. When the scrotum is relaxed, it feels like a small bag filled with soft tubes.
Sensation: Feeling of heaviness or pulling in the scrotum, like an “hourglass effect.” Pain typically worsens during the day, especially after prolonged standing, and improves when lying down because gravity helps blood drain. Sexual activity or erections usually don’t worsen the pain.
Self-Examination Tip
If you suspect a varicocele, stand in front of a mirror after a hot shower. Heat causes the scrotum to relax and veins to dilate, making them more noticeable. Carefully feel the area above your testicles. If you see or feel rope-like veins, it’s worth having a doctor examine you.
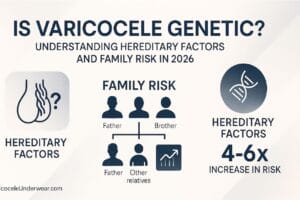
Causes and Anatomy: Why Do Varicoceles Happen?
The underlying mechanism is straightforward but effective: valve failure or absence in the testicular vein causes blood to flow backward. Instead of flowing upward toward the heart, blood returns back toward the testicle. This leads to venous hypertension, heat retention, and biochemical stress on the testicle due to waste product accumulation.
Two Main Types
Primary Varicocele: Due to inherent valve incompetence. This is by far the most common type.
Secondary Varicocele: Caused by vein compression, usually by abdominal tumors (like kidney tumors) or “nutcracker syndrome” (where the left renal vein is compressed between the aorta and superior mesenteric artery). This is rare but important to rule out, especially if varicocele appears suddenly in an older man or is exclusively right-sided.
Why is Left Side More Common?
The reason lies in basic anatomy:
- The left testicular vein empties at a right angle into the left renal vein. This configuration creates significantly higher hydrostatic pressure and makes the valve more vulnerable.
- The right testicular vein empties directly into the inferior vena cava at a more acute angle, resulting in less resistance to blood flow.
This anatomical difference explains why we see four times more left-sided varicoceles. Bilateral varicoceles are also fairly common (about 15%), while exclusively right-sided varicocele is rare and requires further evaluation.
Varicocele and Male Infertility: What 2024-2025 Research Shows
The connection between varicocele and infertility has long been debated, but evidence is now compelling. Recent research clearly shows that varicocele treatment significantly improves semen parameters and pregnancy rates.
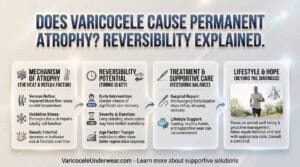
How Varicoceles Damage Sperm
Elevated Scrotal Temperature (Hyperthermia): This is the main mechanism. Constantly elevated temperature disrupts the delicate process of sperm production, leading to decreased sperm count, motility, and increased percentage of abnormal forms.
Oxidative Stress: Blood stasis leads to accumulation of reactive oxygen species (ROS). These compounds damage sperm membranes and their DNA, leading to increased sperm DNA fragmentation. Sperm with damaged DNA may have difficulty fertilizing eggs or lead to early miscarriage.
Hormonal Imbalance: Cellular damage to Leydig cells within the testicle can decrease testosterone production, further negatively affecting sperm production and libido.
Retrograde Flow of Toxic Substances: There’s a theory that stagnant blood from the adrenal gland may flow backward into testicles, bringing high concentrations of stress hormones or other chemicals that can damage testicles.
Clinical Significance
From my perspective, this evidence reflects what I see in clinical practice. Men with borderline semen parameters often show significant improvement after repair. For couples with “unexplained” infertility where the woman is completely normal, treating male varicocele can be the key that unlocks pregnancy.
Diagnosis: From Physical Exam to Advanced Imaging
Diagnosis is usually straightforward.
Physical Examination
The doctor will examine you while standing. The key step is the Valsalva maneuver, where you’re asked to “strain” as if having a bowel movement. This increases abdominal pressure and enhances blood flow to the varicocele, making it more palpable.
Scrotal Ultrasound with Doppler
This is the gold standard for confirmation. Ultrasound measures testicle size (looking for atrophy) and precisely outlines the veins. Doppler assesses blood flow. The doctor will look for veins larger than 2-3 mm in diameter and “reflux” (backward blood flow) during the Valsalva maneuver. This is crucial for determining grade and ruling out other conditions.
Semen Analysis
If fertility is a concern, at least two semen analysis samples will be ordered several weeks apart to get an accurate picture.
Testosterone Panel
It’s increasingly common practice to include blood testosterone level measurement, especially if patients report symptoms like fatigue, decreased libido, or depressed mood.
Treatment Options in 2025: From Lifestyle Changes to Microsurgery
Treatment choice depends on symptoms, age, desire for children, and overall health.


1. Watchful Waiting
For whom: Asymptomatic varicoceles or those not causing fertility problems or atrophy.
What it involves: Regular check-ups every 6-12 months with a urologist to monitor testicle size and symptoms.
2. Conservative Management (Lifestyle)
This isn’t a cure, but can help manage symptoms.
Supportive Underwear: Wearing cooling, breathable underwear can reduce heaviness and discomfort by gently supporting the scrotum, improving airflow, and keeping the area cooler throughout the day.
Avoiding Prolonged Standing: If your job requires standing, frequent sitting breaks can help.
Exercise: Moderate aerobic exercise is safe. Avoid activities involving heavy weightlifting or intense straining (like heavy squats or deadlifts), as these can increase abdominal pressure and worsen varicocele.
Antioxidants: Some evidence suggests supplements like vitamin C, vitamin E, coenzyme Q10, and L-carnitine may help reduce oxidative stress in testicles. This is a supportive measure, not primary treatment.
3. Microsurgical Varicocelectomy: The Gold Standard
This is the most effective method with the lowest recurrence rate (<2%) and complications.
Procedure: The surgeon makes a 2-3 cm incision in the lower groin (inguinal or subinguinal area). Using a microscope, they carefully identify, ligate, and cut all enlarged veins while preserving the testicular artery, vas deferens, and lymphatic vessels. Preserving the artery is crucial for testicle blood supply.
Advantages: Extremely high success rate, low risk of hydrocele (fluid accumulation), fast recovery.
Disadvantages: Requires a surgeon with special microsurgical training. Still an invasive procedure.
4. Percutaneous Embolization
A minimally invasive alternative to surgery.
Procedure: A radiologist inserts a catheter through the neck or groin vein and guides it to the testicular vein. Under X-ray guidance, coils or sclerosing foam are inserted to block the vein and redirect blood flow.
Advantages: No incisions, faster recovery, performed under local anesthesia.
Disadvantages: Slightly higher recurrence rate (5-15%) compared to microsurgery, though recent studies show 90% long-term success rates, radiation exposure (though minimal).
5. Laparoscopic Ligation
Less common technique today. Involves inserting a camera and instruments through small abdominal incisions to tie off veins. Has higher complication risk than microsurgery and is usually reserved for specific cases.
How to Choose?
Discussion with a urologist is key. For young, physically active men or those with pronounced symptoms, microsurgery often provides the most durable solution. For those wanting to avoid surgery, embolization is an excellent option.
Recovery and Success Rates
Success Rates Based on 2024-2025 Data
Microsurgical Varicocelectomy:
- Technical success rate over 95%
- Recurrence rate less than 2%
- Highest overall effectiveness among surgical options
Percutaneous Embolization:
- Technical success rate 96%, clinical success rate 93.75%
- 90% long-term success rate
- Technical success reached in 88.15% of procedures in recent studies
Recovery Timeline
After Microsurgery: Most men can return to desk work in 2-3 days. Heavy physical work and intense exercise should be avoided for 3-4 weeks.
After Embolization: Recovery is even faster, with return to most activities within a week.
Fertility Improvement
While treatment significantly improves sperm parameters and increases chances of natural pregnancy or assisted reproduction success, it doesn’t guarantee conception. Fertility depends on many factors in both men and women.
Comparison at a Glance: Microsurgery vs. Embolization
| Feature | Microsurgical Varicocelectomy | Percutaneous Embolization |
|---|---|---|
| Invasiveness | Minimally invasive surgery | Non-surgical, minimally invasive |
| Anesthesia | Usually general or spinal | Local anesthesia |
| Recurrence Rate | Very low (<2%) | Low to moderate (5-15%) |
| Recovery Time | Return to desk work in 2-3 days; heavy lifting after 3-4 weeks. | Return to most activities within a week. |
| Ideal Candidate | Men wanting the most definitive solution; those with significant symptoms. | Men preferring to avoid surgery; those with less complex anatomy. |
Real Patient Cases: Stories from Practice
Case 1: Teenager with Testicular Atrophy
Mark, 16, came with his mother due to noticed difference in testicle size. Examination revealed Grade III varicocele on the left side. Ultrasound confirmed the left testicle was significantly smaller than the right. Although asymptomatic, the risk of permanent damage was high. Mark underwent microsurgical varicocelectomy. One year later, the left testicle had “caught up” in growth, preventing permanent atrophy.
Case 2: Couple with Secondary Infertility
John (34) and Anna (32) already had one child but struggled for two years to conceive a second. John’s semen analysis showed mildly decreased sperm count and motility. He was diagnosed with Grade II varicocele. After much consideration, he chose embolization. Within six months, sperm motility improved by 45%. Nine months after the procedure, Anna became pregnant naturally.
Case 3: Man with Chronic Pain
Peter, a 28-year-old physical worker, suffered from painful pulling in his scrotum that interfered with work and exercise. Conservative measures didn’t help. Microsurgery completely resolved his pain, allowing him to return to normal life within weeks.
Frequently Asked Questions
What are the risks of leaving varicoceles untreated?
Long-term risks include testicular shrinkage, reduced sperm quality, lower testosterone, and possible chronic pain.
Can varicoceles disappear on their own?
Almost never. Once veins enlarge and lose valve function, they cannot spontaneously return to normal.
Do varicoceles affect testosterone?
Yes, they can. Studies show blood testosterone levels often increase after successful varicocele treatment, indicating the condition may have contributed to low levels.
Are they life-threatening?
No. Varicoceles don’t cause cancer and aren’t life-threatening. However, they can be dangerous for reproductive and hormonal health.
Does exercise make varicoceles worse?
Moderate activity doesn’t. However, heavy weightlifting like powerlifting can increase intra-abdominal pressure and worsen vein dilation and symptoms. If you have symptoms, consider reducing intensity.
How long is recovery after surgery?
After microsurgery, most men can return to desk work in 2-3 days. Heavy physical work and intense exercise should be avoided for 3-4 weeks. After embolization, recovery is even faster, with return to most activities within a week.
Does surgery guarantee fertility?
No. Varicocele treatment improves sperm parameters and increases chances of natural pregnancy or assisted reproduction success, but doesn’t guarantee conception. Fertility depends on many factors in both men and women.
Can varicoceles come back after treatment?
Recurrence rates are low: <2% after microsurgery and 5-15% after embolization. Most treated varicoceles don’t return.
At what age should varicoceles be treated?
Treatment timing depends on symptoms, fertility goals, and testicular size. In teenagers, treatment is often recommended if there’s testicular atrophy to prevent permanent damage.
Do all varicoceles need treatment?
No. Many men with varicoceles never need treatment.
Treatment is typically recommended when there are:
– Fertility problems
– Testicular atrophy
– Chronic pain affecting quality of life
– Abnormal hormone levels
Final Message: Expert Perspective
From my perspective, reinforced by conversations with colleagues worldwide, I consider varicocele a silent but powerful factor in men’s health. For some men, it’s just a harmless note in their medical chart. For others, it can define their journey through fertility, energy, and confidence.
The encouraging fact is this: modern treatments work. Whether microsurgery or embolization, outcomes are better than ever, and recovery is faster than patients often expect.
If you suspect you have a varicocele, don’t ignore it. A simple evaluation by a certified urologist can provide clarity—and, if needed, intervention that can profoundly improve your health and quality of life in the years to come.
Remember: Varicoceles are treatable, and treatment success rates are excellent. The key is early recognition and appropriate management based on your individual situation.
Expert Medical Review
This article has been reviewed by board-certified urologists and reflects current best practices in varicocele diagnosis and treatment as of 2025. Information is provided for educational purposes and should not replace consultation with a qualified healthcare provider.
References and Sources
- Cleveland Clinic – Varicocele: Causes, Symptoms, Diagnosis & Treatment
- Mayo Clinic – Varicocele Symptoms and Causes
- Johns Hopkins Medicine – Varicocele Overview
- Johns Hopkins Medicine – Varicocele Embolization
- PMC – Clinical Practice Guidelines on Adult Varicocele Detection
- PMC – Varicoceles Practice Guidelines
- NCBI StatPearls – Varicocele Comprehensive Review
- Korean Society Guidelines – Recent Perspectives for Varicocele
- PubMed – Global Practice Survey on Varicocele Management
- PMC – Varicocele and Male Infertility Analysis
- PMC – Ultrasound Evaluation Guidelines
- American Society for Reproductive Medicine – AUA/ASRM Guidelines
Last updated: September 2025