The surgery is done, but now you’re facing an unexpected challenge: how do you actually get comfortable enough to sleep? If you just had a varicocelectomy (surgical repair of swollen veins in the scrotum), you’re likely dealing with swelling, tenderness, and real uncertainty about which positions are safe.
Here’s the reality: sleep quality directly affects how fast you heal. Your body repairs tissue and reduces inflammation most effectively during deep rest. But the wrong position can increase scrotal pressure, worsen swelling, or strain your incision.
This guide covers exactly how to sleep during each phase of your first week. You’ll learn which positions speed recovery, which to avoid, and practical adjustments from clinical experience. For a full overview of varicocele causes, symptoms, and treatment options, see our complete varicocele guide.
Why Does Sleep Position Matter After Varicocelectomy?
Your sleeping position affects three critical factors during varicocelectomy recovery:
| Factor | How Position Affects It |
|---|---|
| Blood flow | Proper positioning promotes venous drainage away from the surgical site |
| Swelling | Gravity can reduce or worsen scrotal edema based on position |
| Incision stress | Certain movements put tension on stitches, risking wound complications |
According to post-operative care guidelines, varicocelectomy success rates exceed 90% when patients follow proper recovery protocols. Sleep positioning is often overlooked, yet it affects both comfort and healing speed.
The surgical site remains vulnerable during the first 7 days. Internal sutures need time to hold, and tissue needs reduced pressure to heal properly. Getting this right matters more than most patients realize.
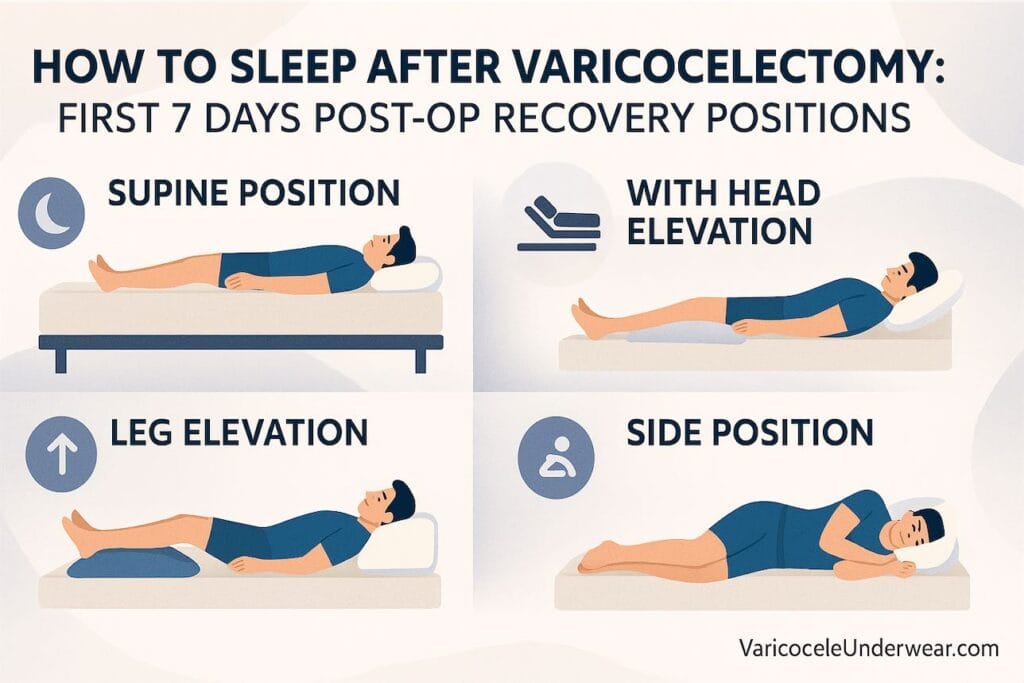
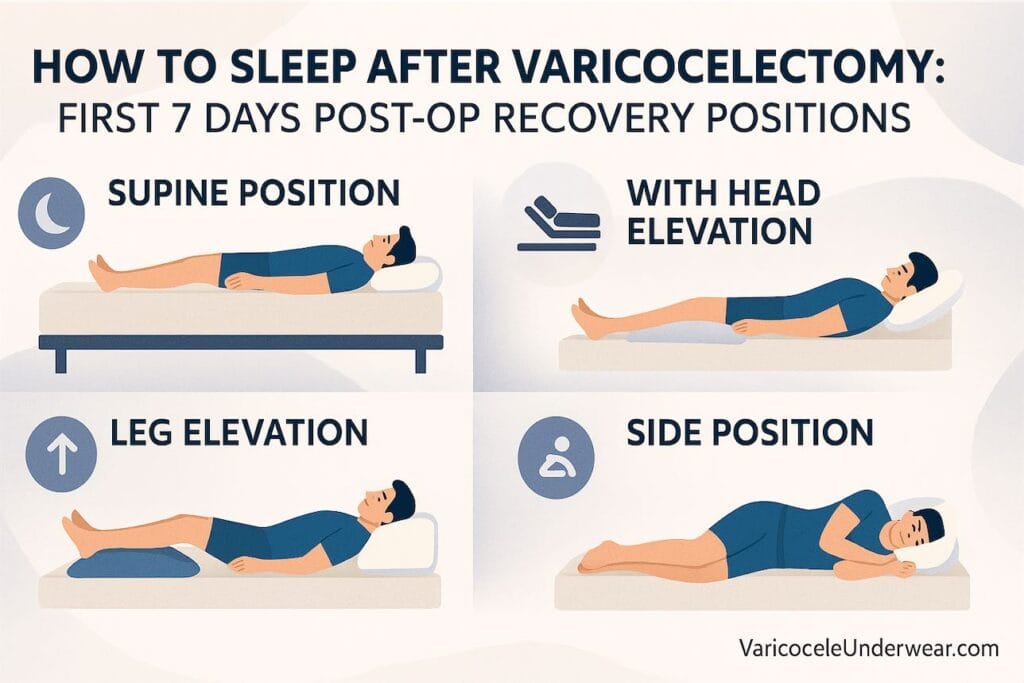
Best Sleeping Position After Varicocelectomy Surgery
The gold standard: Back sleeping with slight leg elevation.
This position offers three key benefits:
- Minimizes scrotal pressure by keeping weight off the groin
- Promotes blood return to the heart, reducing swelling
- Keeps the incision site stable without stretching or compression
How to Set Up the Ideal Position
- Place a pillow under your knees to reduce lower back strain
- Use a small, rolled towel under the scrotum for gentle support
- Keep your upper body slightly elevated (15-20 degrees) using a wedge pillow or stacked pillows
Pro tip from clinical experience: Many men find hospital-style adjustable beds helpful during recovery. If you don’t have one, a recliner can work well for the first 2-3 nights.
Day-by-Day Sleep Recovery Guide: Days 1-7
Your sleep needs and restrictions change as healing progresses. Here’s what to expect:
Days 1-2: Strict Back Sleeping
The most critical period. Anesthesia effects may still linger, and swelling typically peaks within 48 hours.
Recommendations:
- Sleep only on your back
- Keep the scrotum elevated with a rolled towel
- Ice before bed (20 minutes on, 20 off) to reduce overnight swelling
- Take prescribed pain medication 30 minutes before sleep
Wearing supportive underwear designed for varicocele recovery can reduce nighttime movement and keep ice packs in place.
Days 3-4: Careful Movement Permitted
Swelling should start decreasing. Most men report improved comfort.
Recommendations:
- Continue back sleeping as primary position
- Brief, careful side-lying may be tolerated (see next section)
- Reduce elevation slightly if comfortable
- Continue scrotal support, especially during sleep
Days 5-7: Gradual Position Flexibility
By now, external incisions are closing. Internal healing continues, but position restrictions ease.
Recommendations:
- Side sleeping becomes safe for most patients
- Stomach sleeping still not recommended
- Continue wearing supportive underwear at night
- Watch for position-related pain as a warning sign
Can You Sleep on Your Side After Varicocelectomy?
Short answer: Yes, typically by days 3-5, with modifications.
Side sleeping puts mild lateral pressure on the scrotal area. During the first 48 hours, this can worsen swelling and discomfort. By days 3-4, most men can try side positions if they:
- Place a pillow between the knees
- Use supportive underwear to prevent scrotal movement
- Start with the non-surgical side (if applicable)
- Listen to their body and return to back sleeping if pain increases
Side Sleeping Modification Table
| Day Post-Op | Side Sleeping? | Modifications Needed |
|---|---|---|
| Days 1-2 | Not recommended | N/A |
| Days 3-4 | Cautiously | Pillow between knees, supportive briefs |
| Days 5-7 | Generally safe | Maintain scrotal support |
| Week 2+ | Resume normal | None required |
Case example: A 34-year-old patient who underwent microsurgical varicocelectomy reported that attempting side sleeping on night 2 caused noticeable swelling increase by morning. After switching back to back sleeping with elevation, swelling normalized within 24 hours.
Positions to Avoid During the First Week
Some sleeping positions create problems during early recovery:
Stomach Sleeping
Avoid for at least 2 weeks. This position:
- Puts direct pressure on the surgical site
- Can cause incision irritation
- Increases core temperature around the scrotum, which may affect healing
Fetal Position (Curled Up)
Avoid for 5-7 days. Tight hip flexion:
- Compresses the inguinal region
- May stress incision lines, especially after inguinal approach surgery
- Restricts blood flow to the lower extremities
Elevated Legs Too High
While some elevation helps, raising legs above heart level can:
- Increase blood pressure in the pelvic region
- Potentially stress surgical repairs
- Cause lower back discomfort
How to Set Up Your Bed for Post-Op Recovery
Preparation before surgery makes nighttime recovery much smoother. Consider these adjustments:
Essential Setup:
- Wedge pillow or 2-3 firm pillows for upper body elevation
- Knee pillow to maintain spinal alignment
- Ice packs within arm’s reach (wrapped, not direct contact)
- Phone/remote accessible without stretching
- Water bottle nearby to stay hydrated
Optional But Helpful:
- Recliner in bedroom for first 2 nights
- Bedside urinal to minimize trips to bathroom
- Extra absorbent pad under sheets (for ice pack condensation)
Managing Pain and Discomfort at Night
Sleep disruption is common during the first 3-4 nights. According to Cleveland Clinic guidelines, proper pain management supports healing.
Pain Management Strategies
- Time your medications to peak during sleep hours (take 30-45 minutes before bed)
- Use ice therapy before sleeping to reduce overnight inflammation
- Wear scrotal support to minimize movement that triggers pain
- Limit fluids 2 hours before bed to reduce bathroom trips
When to Contact Your Doctor
Call your surgeon if you experience:
- Pain that suddenly worsens after days 2-3
- Fever above 100.4°F (38°C)
- Significant swelling increase rather than decrease
- Signs of infection at the incision site
When Can You Return to Normal Sleep Positions?
Most patients resume their preferred sleeping positions within 2-3 weeks. The timeline varies based on:
| Surgery Type | Return to Normal Sleep |
|---|---|
| Microsurgical (subinguinal) | 10-14 days |
| Laparoscopic | 7-10 days |
| Open inguinal | 14-21 days |
Research published in the Journal of Urology indicates that microsurgical approaches generally allow faster recovery with lower complication rates. Your specific timeline depends on your surgeon’s technique and how your body responds.
Key indicator: When changing positions no longer causes pain or discomfort, you’re likely ready for normal sleep patterns. Always confirm with your surgeon during follow-up.
Quick Reference: Varicocelectomy Sleep Position Summary
| Recovery Phase | Best Position | Key Support Needed | Watch For |
|---|---|---|---|
| Days 1-2 | Back only, elevated | Scrotal support, ice | Peak swelling |
| Days 3-4 | Back primary, side cautiously | Pillow between knees | Position-related pain |
| Days 5-7 | Back or side | Supportive underwear | Decreasing symptoms |
| Week 2 | Patient preference | Optional support | Full comfort return |
Frequently Asked Questions
How long after varicocelectomy can I sleep on my stomach?
Most urologists recommend waiting at least 2 weeks before stomach sleeping. This position puts direct pressure on the surgical site and can irritate healing incisions. If stomach sleeping is essential for you, try transitioning around day 14 while using a pillow under your hips to reduce groin pressure. Stop immediately if you notice increased swelling or discomfort.
Will sleeping in the wrong position damage my surgery results?
Sleeping in suboptimal positions during the first few days is unlikely to reverse surgical repair, but it can increase swelling, slow healing, and cause unnecessary pain. The veins have been surgically ligated (tied off), so short periods of poor positioning won’t undo the procedure. However, consistent poor positioning can delay your return to normal activities and prolong discomfort.
Should I wear underwear to bed during varicocelectomy recovery?
Yes. Supportive underwear or a scrotal support garment reduces movement and provides gentle compression that minimizes swelling. Many patients find that cooling varicocele support underwear works well for overnight wear because it maintains position without overheating the area. Avoid loose boxers during the first week.
Final Takeaway
Getting quality sleep after varicocelectomy comes down to three principles: back sleeping with elevation for the first 48-72 hours, gradual transition to side sleeping around days 3-5, and consistent scrotal support throughout the first week. Your body does its best repair work during sleep, so protecting this time directly affects how quickly you return to normal life.
If pain or swelling increases rather than decreases after day 3, contact your surgeon. Most men find that by the end of week one, sleep becomes noticeably more comfortable with each passing night.
Have questions about your recovery experience? Share in the comments below, or consult with your urologist for personalized guidance.