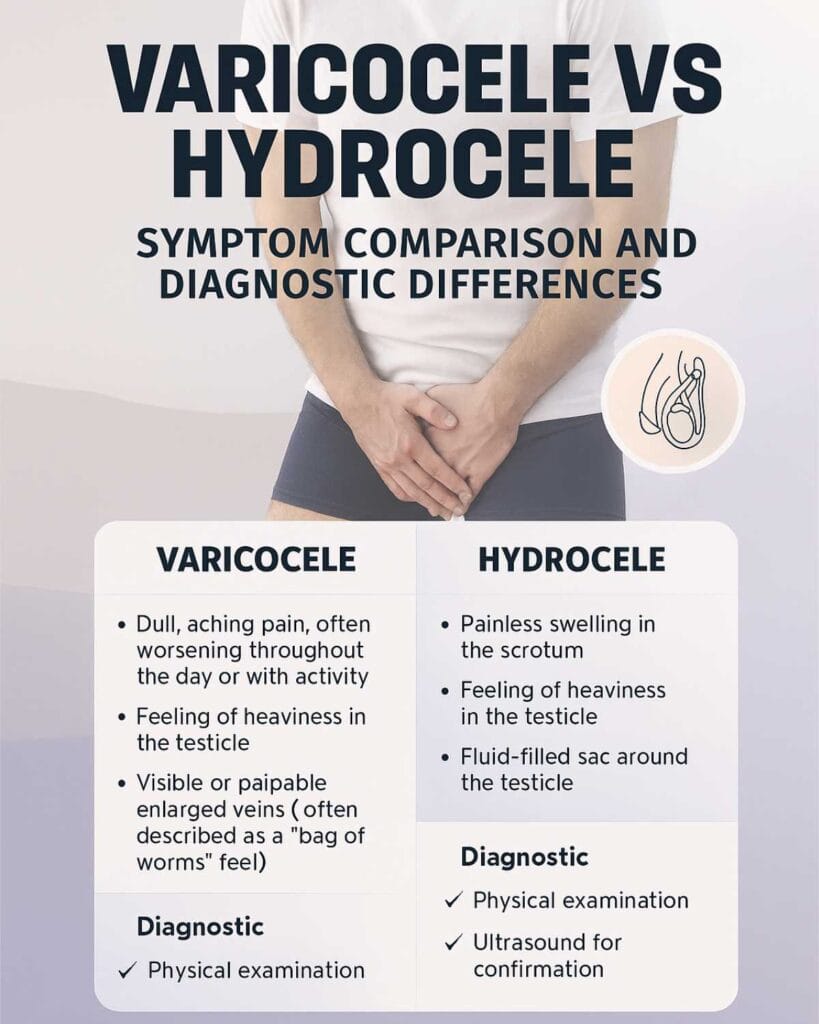
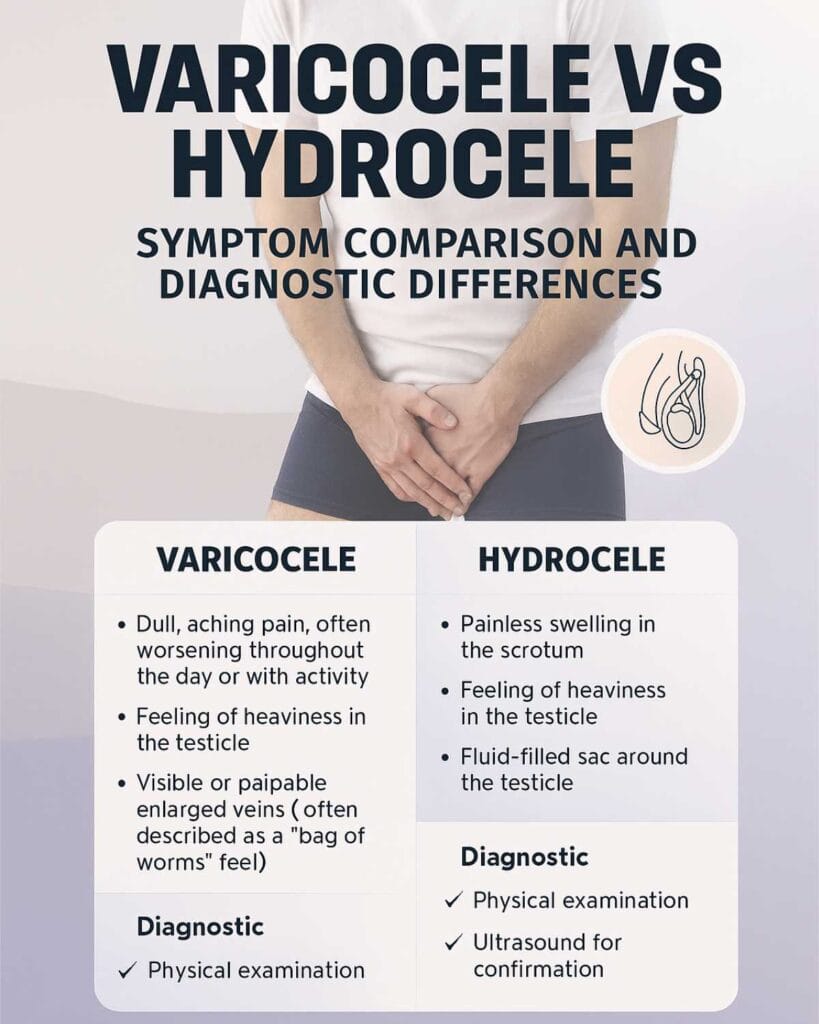
Scrotal swelling affects millions of men worldwide but often stems from two distinct conditions: varicocele and hydrocele. While both cause testicular enlargement, they differ fundamentally in their causes, health implications, and treatment requirements. Varicocele affects approximately 15-20% of all adult males and up to 40% of men experiencing fertility problems. Hydrocele typically causes painless swelling with minimal fertility impact. This guide compares symptoms, diagnostic methods, and treatment options to help you recognize each condition and make informed decisions about your reproductive health.
For men concerned about testicular health and fertility, understanding these conditions is the first step toward appropriate treatment. Learn more about causes, symptoms, and management strategies in this complete varicocele guide. Men experiencing discomfort may find relief through supportive measures like specialized varicocele support underwear that provides targeted compression and cooling.
What Causes Varicocele
Varicocele develops when valves inside the veins of the pampiniform plexus malfunction, allowing blood to pool and veins to enlarge. The condition predominantly affects the left testicle due to anatomical differences. The left testicular vein drains into the left renal vein at a 90-degree angle, creating higher pressure compared to the right side’s direct drainage, which explains why 80-90% of varicoceles occur on the left side.
The enlarged veins create a “bag of worms” texture felt during physical examination. Blood pooling increases scrotal temperature by 1-2 degrees Celsius, which damages sperm production and quality. Additional factors contributing to testicular dysfunction include oxidative stress, hypoxia from venous stasis, and possible reflux of adrenal metabolites into the testicular circulation.
What Causes Hydrocele
Hydrocele forms when fluid accumulates between the layers of the tunica vaginalis, the membrane surrounding the testicle. Two types exist: congenital hydroceles present at birth when the processus vaginalis fails to close properly, and acquired hydroceles that develop after trauma, infection, inflammation, or rarely tumor.
Unlike varicocele’s vascular origin, hydrocele involves serous fluid collection. The fluid-filled sac creates smooth, painless swelling that transilluminates (glows) when light is shined through it. Most adult hydroceles develop gradually without identifiable cause, though up to 5% may develop after varicocele repair surgery.
Symptom Comparison
Varicocele Symptoms
Men with varicocele commonly experience:
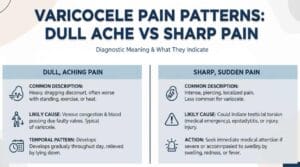
- Dull, aching pain that worsens after prolonged standing or physical activity
- Heavy or dragging sensation in the affected testicle
- Visible or palpable enlarged veins with “bag of worms” appearance
- Testicular shrinkage (atrophy) on the affected side in severe cases
- Symptoms that improve when lying down
Pain occurs in 2-10% of varicocele patients. The discomfort typically radiates from the scrotum to the inguinal region along the spermatic cord path. Many men remain asymptomatic and discover varicocele during fertility evaluation or routine physical examination.
Hydrocele Symptoms
Hydrocele typically presents as:
- Gradual, painless scrotal swelling on one or both sides
- Smooth, fluid-filled sensation without lumps
- Pressure or heaviness without sharp pain
- Swelling that may increase during the day and decrease overnight
- No pain during palpation or movement
Sudden pain with hydrocele warrants immediate medical evaluation as it may indicate infection, bleeding, testicular torsion, or other acute complications requiring urgent treatment.
Diagnostic Methods
Physical Examination
Urologists diagnose both conditions through systematic scrotal examination in standing and lying positions. For varicocele, doctors palpate for enlarged veins and observe how they change with position and Valsalva maneuver (bearing down as if straining). Physical examination alone detects clinically significant varicoceles with approximately 70% sensitivity, missing smaller subclinical cases.
Transillumination helps distinguish hydrocele from solid masses. A bright light shined through the scrotum causes fluid-filled hydroceles to glow brightly, while varicoceles and tumors block light transmission. This simple bedside test provides preliminary screening but cannot replace imaging studies for definitive diagnosis.
Ultrasound and Doppler Imaging
Color Doppler ultrasound is the diagnostic gold standard for both conditions, achieving 92-95% sensitivity for varicocele detection. The imaging visualizes blood flow direction and identifies venous reflux during Valsalva maneuver. Varicocele diagnosis requires veins exceeding 2-3 mm diameter with reverse blood flow.
For hydrocele evaluation, ultrasound shows echo-free fluid collection between tunica vaginalis layers while ruling out underlying testicular masses or other pathology. Ultrasound also measures testicular volume, detects subclinical varicoceles, assesses blood flow patterns, and identifies concurrent conditions affecting both testicles simultaneously.
Fertility Impact
How Varicocele Affects Fertility
Varicocele is present in 35-40% of men with primary infertility. The condition impairs fertility through multiple mechanisms including elevated testicular temperature, oxidative stress from increased reactive oxygen species, venous stasis causing hypoxia, and potential reflux of adrenal metabolites.
Research demonstrates significant improvement after varicocele repair. Meta-analyses show sperm count increases by 9.71-12.32 million/mL, motility improves by 10.86%, and morphology by 9.69% following surgical correction. Men with initial sperm counts above 8 million/mL and progressive motility above 18% experience the most substantial improvements after surgery.
| Fertility Parameter | Impact of Untreated Varicocele | Improvement After Repair |
|---|---|---|
| Sperm count | Reduced 30-50% | Increases 9.71-12.32 million/mL |
| Sperm motility | Decreased progressive movement | Improves by 10.86% |
| Sperm morphology | Abnormal forms increase | Improves by 9.69% |
| DNA fragmentation | Elevated oxidative damage | Reduces significantly |
| Pregnancy rates | Reduced natural conception | Improves 40-60% |
How Hydrocele Affects Fertility
Hydrocele rarely interferes with fertility unless the condition becomes large enough to compress testicular tissue or impair blood supply. Most hydroceles remain benign with no direct effect on sperm production, quality, or male reproductive function. Large hydroceles may cause discomfort or cosmetic concerns but typically do not require fertility-focused treatment.
Treatment Options
Varicocele Treatment
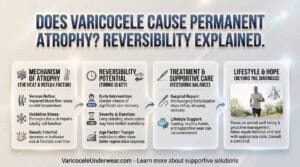
Treatment becomes medically appropriate when varicocele causes persistent pain, testicular atrophy, abnormal semen parameters in men seeking fertility, or progressive testicular damage. Surgical options include microsurgical varicocelectomy (considered the gold standard), laparoscopic varicocelectomy, and open retroperitoneal approaches.
Percutaneous embolization achieves 90-97% technical success with recurrence rates between 2-24%, comparable to surgical outcomes. Both interventions demonstrate similar improvements in semen parameters and pregnancy rates. The procedure involves threading a catheter through the femoral vein to the spermatic vein and blocking blood flow with coils or sclerosing agents.
Conservative management includes:
- Supportive underwear with targeted compression
- Anti-inflammatory medication for pain control
- Ice application for acute discomfort
- Avoiding prolonged standing or heavy lifting
Semen analysis performed 4 months after treatment typically shows improvement, with pregnancy rates increasing by 30-50% in couples where male factor infertility was the primary concern.
Hydrocele Treatment
Small, asymptomatic hydroceles require no treatment, only periodic monitoring. Surgical intervention (hydrocelectomy) becomes appropriate when hydrocele causes significant discomfort, interference with daily activities, cosmetic concerns, or rapid size increase. The procedure involves draining fluid and closing the communication between the abdominal cavity and scrotum for communicating hydroceles.
Needle aspiration provides temporary relief but carries high recurrence risk (80-90%). Sclerotherapy, injecting irritating agents after aspiration, reduces recurrence but may cause inflammation and infection. Surgical excision remains the definitive treatment with recurrence rates below 5%.
When to See a Doctor
Seek medical evaluation for:
- New scrotal swelling or lumps, regardless of pain level
- Gradual testicular enlargement or asymmetry
- Persistent scrotal aching or heaviness
- Fertility concerns with scrotal abnormalities
- Sudden, severe testicular pain (medical emergency)
Early diagnosis prevents complications and preserves fertility potential. Both conditions require professional assessment through physical examination and imaging studies. Self-diagnosis cannot replace clinical evaluation by a qualified urologist or men’s health specialist.
Risk Factors and Prevention
Varicocele Risk Factors
Varicocele typically develops during puberty when testicular blood flow increases significantly. Risk factors include:
- Age 15-25 years (peak development period)
- Left-sided anatomical predisposition
- Family history of varicocele
- Tall stature and rapid growth
No proven prevention methods exist, though maintaining healthy body weight and avoiding prolonged increases in abdominal pressure may reduce risk.
Hydrocele Risk Factors
Acquired hydroceles develop more commonly in men over 40 years old. Risk factors include:
- Previous scrotal trauma or surgery
- Infections such as epididymitis or sexually transmitted infections
- Testicular cancer or other tumors
- Inflammatory conditions affecting the scrotum
Preventing trauma and promptly treating infections may reduce hydrocele risk, though many cases develop without identifiable causes.
FAQ
Can varicocele and hydrocele occur together?
Yes, both conditions can coexist in the same patient. Research indicates 20-25% of varicocele surgeries involve concurrent patent internal inguinal rings, which may contribute to hydrocele formation. Physical examination and ultrasound distinguish between the two conditions when present simultaneously.
Does varicocele always require surgery?
No. Treatment depends on symptom severity, fertility goals, and testicular damage evidence. Men with mild, asymptomatic varicoceles and normal semen parameters may opt for conservative management with supportive underwear and monitoring. Surgery becomes necessary for pain, fertility issues, or testicular atrophy.
How accurate is physical examination compared to ultrasound?
Physical examination detects varicoceles with approximately 70% sensitivity, while Doppler ultrasound achieves 92-95% sensitivity. Ultrasound identifies subclinical (non-palpable) varicoceles and provides detailed information about venous reflux, testicular size, and blood flow patterns that physical examination cannot assess.