If you’ve noticed a dull ache in your scrotum, a feeling of heaviness that worsens throughout the day, or you’re concerned about fertility issues, you may be dealing with a varicocele. This common vascular condition affects approximately 15% of all men and up to 40% of men experiencing infertility, yet many suffer in silence, unsure whether treatment is necessary or what options exist.
As a men’s health specialist, I understand the anxiety and confusion that comes with a varicocele diagnosis. You’re likely wondering: Do I need surgery? Will this affect my ability to have children? What’s the recovery like? This comprehensive guide will walk you through everything you need to know about varicocele treatment in 2026—from conservative management to surgical interventions, success rates, and what to expect during recovery.
Whether you’ve just been diagnosed or you’re exploring treatment options, this article provides evidence-based information to help you make informed decisions about your health. We’ll cover when treatment is necessary, the most effective approaches available today, and how to optimize your recovery for the best possible outcomes.
What Is a Varicocele and Why Does It Need Treatment?
A varicocele is an enlargement of the veins within the scrotum, similar to varicose veins that can occur in the legs. These veins, part of the pampiniform plexus, normally transport blood away from the testicles. When the valves inside these veins malfunction, blood pools and causes the veins to swell, creating a varicocele.
The Clinical Impact
The condition typically develops during puberty and affects the left testicle in 90% of cases due to anatomical differences in venous drainage. While some men experience no symptoms, others face:
- Chronic discomfort: Dull, aching pain that worsens with standing or physical activity
- Testicular atrophy: The affected testicle may become smaller due to impaired blood flow
- Fertility problems: Elevated scrotal temperature and oxidative stress can damage sperm production
- Hormonal imbalance: Reduced testosterone levels in some cases
When Treatment Becomes Necessary
Not every varicocele requires intervention. According to the American Urological Association guidelines, treatment should be considered when:
- Fertility is compromised: Abnormal semen parameters with a documented varicocele
- Pain is present: Persistent discomfort that affects quality of life
- Testicular atrophy occurs: Progressive size difference between testicles exceeding 20%
- Adolescent cases: When there’s evidence of impaired testicular growth
Research published in the Journal of Urology demonstrates that approximately 60-80% of men with varicoceles maintain normal fertility, suggesting that observation without treatment is appropriate for asymptomatic cases.
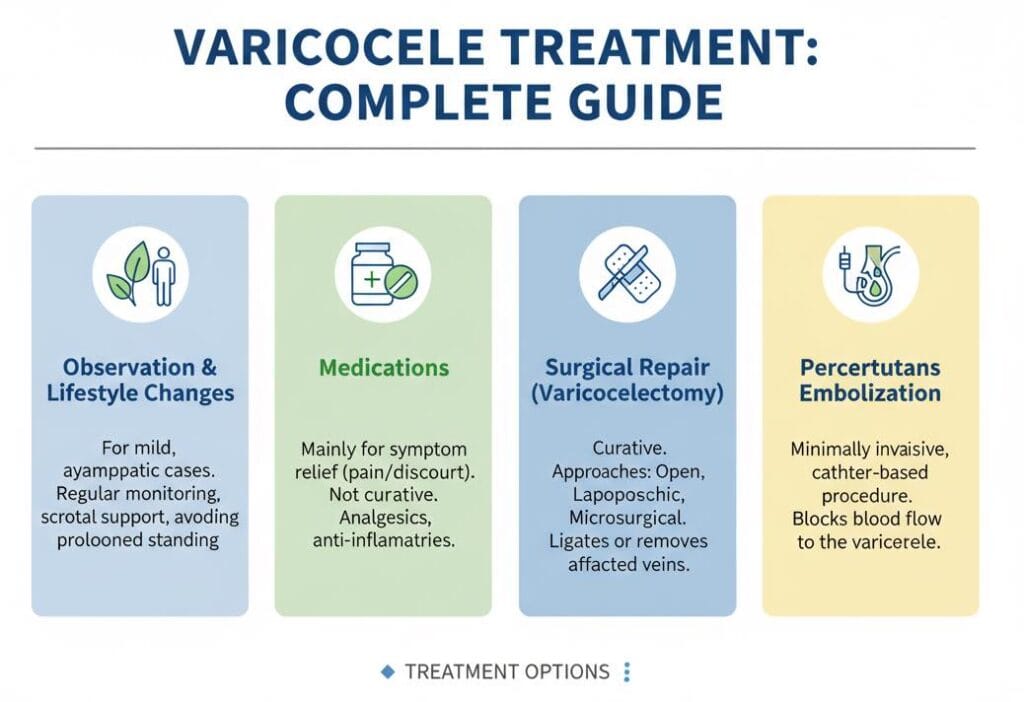
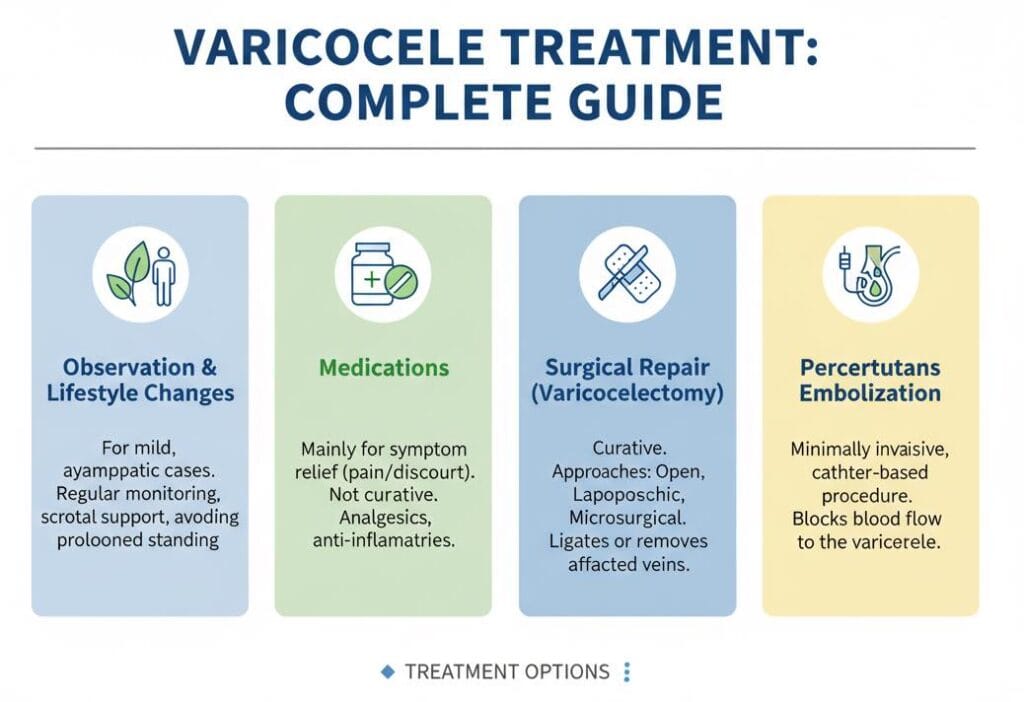
Conservative Management: Non-Surgical Treatment Options
Before considering surgical intervention, many men benefit from conservative approaches that can reduce symptoms and improve comfort.
Supportive Underwear and Lifestyle Modifications


Specialized support garments have emerged as an effective first-line approach for symptom management. Supportive underwear designed specifically for varicoceles provides gentle elevation and cooling properties that can:
- Reduce venous pooling by supporting the scrotum
- Lower scrotal temperature through breathable, moisture-wicking fabrics
- Minimize discomfort during daily activities
- Provide an alternative for men who want to avoid or delay surgery
Clinical insight: In my practice, I recommend supportive underwear as a first-line intervention for men with grade 1-2 varicoceles who experience mild to moderate discomfort. Many patients report significant symptom improvement within 2-4 weeks of consistent use.
Pain Management Strategies
For men experiencing varicocele-related discomfort:
- NSAIDs: Over-the-counter anti-inflammatory medications (ibuprofen, naproxen) can reduce pain and inflammation
- Ice therapy: Applying cold packs for 15-20 minutes several times daily helps reduce swelling
- Activity modification: Avoiding prolonged standing and heavy lifting minimizes venous congestion
- Scrotal elevation: Lying down with the pelvis elevated promotes venous drainage
Supplements and Oxidative Stress Reduction
Research in Fertility and Sterility indicates that varicoceles create oxidative stress that damages sperm DNA. Antioxidant supplementation may help:
- Vitamin C and E: 500-1000mg daily of combined antioxidants
- Coenzyme Q10: 200-300mg daily supports mitochondrial function
- L-carnitine: 2-3g daily may improve sperm motility
- Zinc and selenium: Essential minerals for sperm health
Important note: Supplements support but don’t replace treatment when varicoceles cause significant fertility issues or pain. Always consult with your healthcare provider before starting any supplement regimen.
When Conservative Management Isn’t Enough
While these approaches provide relief for many men, they don’t address the underlying vascular problem. If symptoms persist after 3-6 months of conservative management, or if fertility parameters continue to decline, surgical intervention should be considered.
Surgical Treatment Options: Comprehensive Overview
Modern varicocele surgery aims to redirect blood flow away from the enlarged veins while preserving the testicular artery and lymphatic vessels. Four main surgical approaches are available in 2026, each with distinct advantages and considerations.
1. Microsurgical Varicocelectomy (Subinguinal Approach)
This is considered the gold standard for varicocele repair, performed through a small incision in the groin area below the inguinal canal.
Procedure details:
- Performed under general or regional anesthesia
- Uses surgical microscope (16-25x magnification) to identify and ligate affected veins
- Preserves testicular artery and lymphatic vessels with precision
- Outpatient procedure taking 60-90 minutes
Success rates and outcomes:
According to meta-analysis data published in Asian Journal of Andrology:
- Recurrence rate: 1-2% (lowest among all techniques)
- Hydrocele formation: Less than 1%
- Semen improvement: 60-70% of men show significant improvement
- Pregnancy rates: 40-50% achieve pregnancy within 12-18 months post-surgery
Advantages:
- Highest success rate with lowest complication risk
- Excellent visualization of all anatomical structures
- Minimal postoperative pain
- Fastest recovery time
Disadvantages:
- Requires specialized training and equipment
- Slightly longer operative time
- May not be available at all centers
Patient experience: In my surgical practice, microsurgical varicocelectomy has become my preferred approach. A 32-year-old patient with a grade 3 varicocele and poor sperm motility underwent this procedure. His sperm concentration increased from 8 million/mL to 35 million/mL within six months, and his partner conceived naturally at nine months post-surgery.
2. Laparoscopic Varicocelectomy
A minimally invasive approach using small abdominal incisions and a camera to visualize and ligate the spermatic veins.
Procedure details:
- Requires general anesthesia
- Three small incisions (5-10mm) in the lower abdomen
- Carbon dioxide gas inflates the abdomen for visualization
- Veins are clipped or cauterized at the internal inguinal ring level
- Duration: 45-75 minutes
Success rates and outcomes:
Clinical data from European Urology reports:
- Recurrence rate: 3-5%
- Hydrocele formation: 3-7%
- Semen improvement: 50-65% of patients
- Complication rate: 2-8% (higher than microsurgical approach)
Advantages:
- Bilateral varicoceles can be addressed simultaneously
- Good cosmetic results with small scars
- Effective for recurrent varicoceles
Disadvantages:
- Requires general anesthesia
- Longer recovery than microsurgical approach
- Risk of intra-abdominal complications (rare)
- Higher hydrocele risk due to lymphatic vessel injury
3. Open Surgical Varicocelectomy (Inguinal/Retroperitoneal)
Traditional surgical approach through a larger incision in the groin (inguinal) or lower abdomen (retroperitoneal).
Procedure details:
- Local, regional, or general anesthesia options
- 3-5cm incision to access spermatic cord
- Veins ligated without microscopic magnification
- Can be performed in resource-limited settings
Success rates and outcomes:
Systematic review data indicates:
- Recurrence rate: 5-15%
- Hydrocele formation: 7-15%
- Arterial injury risk: 1-5%
- Semen improvement: 40-60% of patients
Advantages:
- Widely available technique
- Lower cost compared to microsurgical or laparoscopic approaches
- Can be performed under local anesthesia
Disadvantages:
- Higher recurrence and complication rates
- More postoperative pain
- Longer recovery period (2-3 weeks)
- Greater risk of arterial and lymphatic injury
4. Percutaneous Embolization
A non-surgical, interventional radiology procedure that blocks varicocele veins from the inside using coils or sclerosing agents.
Procedure details:
- Performed under local anesthesia with conscious sedation
- Catheter inserted through femoral or jugular vein
- Guided by fluoroscopy to the affected testicular vein
- Coils or sclerosant injected to block blood flow
- Duration: 30-60 minutes
Success rates and outcomes:
According to research in CardioVascular and Interventional Radiology:
- Technical success rate: 90-95%
- Recurrence rate: 10-15%
- Hydrocele formation: Rare (less than 1%)
- Semen improvement: 50-60% of patients
- Complication rate: 5-10%
Advantages:
- No surgical incision required
- Can be performed as outpatient procedure
- Immediate return to normal activities
- Bilateral treatment possible in one session
Disadvantages:
- Higher recurrence rate than surgical options
- Risk of coil migration (rare)
- Venous perforation or thrombosis (1-3%)
- Not suitable for all anatomical variations
- Limited long-term data compared to surgical approaches
Treatment Comparison Table
| Approach | Recurrence Rate | Hydrocele Risk | Recovery Time | Anesthesia | Cost |
|---|---|---|---|---|---|
| Microsurgical | 1-2% | <1% | 1-2 weeks | General/Regional | $$$ |
| Laparoscopic | 3-5% | 3-7% | 2-3 weeks | General | $$$ |
| Open Surgical | 5-15% | 7-15% | 2-4 weeks | Local/General | $$ |
| Embolization | 10-15% | <1% | 3-7 days | Local/Sedation | $$$ |
Who Should Consider Varicocele Treatment?
Clinical decision-making for varicocele treatment has evolved significantly with updated guidelines from major urological organizations. The decision isn’t always straightforward and requires careful evaluation of multiple factors.
Fertility-Related Indications
The American Society for Reproductive Medicine (ASRM) recommends varicocele repair when:
- Abnormal semen parameters are present: Total motile sperm count below 5-10 million
- Couple has documented infertility: Unable to conceive after 12 months of unprotected intercourse
- Palpable varicocele exists: Grade 2 or 3 varicocele on physical examination
- Female partner has normal fertility: Or treatable fertility issues
Evidence-based outcomes: A landmark meta-analysis in Cochrane Database of Systematic Reviews examining 10 randomized controlled trials found that varicocele repair in subfertile men improved pregnancy rates (OR 2.39, 95% CI 1.56-3.66) compared to observation alone.
Pain-Related Indications
Approximately 2-10% of men with varicoceles experience chronic scrotal pain. Treatment is indicated when:
- Pain persists for more than 3 months
- Conservative measures have failed
- Pain significantly impacts quality of life
- Physical examination confirms varicocele as the pain source
Clinical pearl: I’ve observed that men with grade 2-3 varicoceles report pain relief rates of 70-90% following microsurgical repair, with most experiencing improvement within 4-8 weeks post-surgery.
Adolescent Varicoceles
Treatment in adolescents requires special consideration. The Pediatric Urology guidelines suggest intervention when:
- Testicular volume discrepancy: Greater than 20% difference or 2mL absolute difference
- Progressive testicular hypotrophy: Documented shrinkage over time
- Bilateral palpable varicoceles: Especially high-grade
- Adolescent requests treatment: For symptoms or psychological concerns
Long-term considerations: Studies in The Journal of Urology demonstrate that 70-80% of adolescents with testicular volume asymmetry achieve catch-up growth following varicocelectomy, with maximum benefit occurring when treated before age 18.
Testosterone Deficiency
Emerging research suggests varicoceles may impact testosterone production. A 2021 study in The World Journal of Men’s Health found that:
- Men with varicoceles had significantly lower testosterone levels (mean 385 ng/dL) compared to controls (mean 450 ng/dL)
- Varicocele repair increased testosterone by an average of 97 ng/dL
- Improvement was most significant in men with baseline testosterone below 300 ng/dL
Clinical application: While testosterone improvement shouldn’t be the sole indication for surgery, men with symptomatic hypogonadism and palpable varicoceles may benefit from repair as part of comprehensive management.
When Observation Is Appropriate
Not every varicocele requires treatment. Conservative management with monitoring is suitable for:
- Asymptomatic men with normal semen parameters
- Grade 1 varicoceles without fertility concerns
- Men who have completed their families and have no symptoms
- Cases where female factor infertility is the primary issue
Case study: A 28-year-old patient with a grade 2 left varicocele, no pain, and normal semen analysis (concentration: 42 million/mL, motility: 55%) chose observation. After two years of monitoring with annual semen analyses, his parameters remained stable, and he successfully fathered two children naturally.
Pre-Operative Preparation and What to Expect
Proper preparation optimizes surgical outcomes and reduces anxiety. Here’s what you need to know before undergoing varicocele repair.
Initial Consultation and Diagnostic Workup
Physical examination:
- Performed standing and lying down
- Valsalva maneuver (bearing down) accentuates varicocele
- Grading: Grade 1 (palpable with Valsalva), Grade 2 (palpable without Valsalva), Grade 3 (visible)
Semen analysis:
- Minimum two samples, 2-7 days apart
- 2-5 days of abstinence before collection
- Parameters assessed: concentration, motility, morphology, volume
Scrotal ultrasound:
- Confirms diagnosis when physical exam is unclear
- Measures testicular volume
- Identifies venous diameter (>3mm suggestive of varicocele)
- Rules out other pathology
Hormonal evaluation (selective cases):
- Total and free testosterone
- Luteinizing hormone (LH) and follicle-stimulating hormone (FSH)
- Prolactin and estradiol if indicated
Pre-Operative Instructions
One week before surgery:
- Stop blood-thinning medications (aspirin, ibuprofen, fish oil) as directed
- Avoid herbal supplements that may affect bleeding
- Arrange transportation home after surgery
- Purchase recommended supportive underwear for recovery
Day before surgery:
- Shower using antibacterial soap
- Trim or shave scrotal hair if instructed
- Follow fasting guidelines (typically nothing after midnight)
- Confirm pickup arrangements
Day of surgery:
- Wear comfortable, loose-fitting clothing
- Bring photo identification and insurance information
- Leave valuables at home
- Expect to spend 2-4 hours at the facility
Questions to Ask Your Surgeon
- What is your experience level with this specific technique?
- What are your personal complication and success rates?
- Will you use optical magnification?
- How many veins typically require ligation?
- What type of anesthesia will be used?
- What should I expect for pain management?
- When can I return to work and exercise?
- When should we repeat semen analysis?
The Surgical Experience: Step-by-Step
Understanding what happens during surgery can significantly reduce anxiety. Here’s a detailed walkthrough of microsurgical varicocelectomy, the most commonly recommended approach.
Arrival and Pre-Operative Care
Check-in process (30-60 minutes before surgery):
- Vital signs assessment
- IV line placement
- Final consultation with surgeon and anesthesiologist
- Consent form review
Anesthesia administration:
- General anesthesia: Complete unconsciousness via IV and breathing tube
- Regional anesthesia (spinal/epidural): Numbness from waist down while awake
- Choice depends on surgeon preference and patient factors
The Surgical Procedure
Microsurgical varicocelectomy technique:
- Incision (minutes 0-5):
- Small incision (2-3cm) made just above the scrotum
- Subcutaneous tissues carefully separated
- Spermatic cord exposure (minutes 5-15):
- Surgical microscope positioned
- Spermatic cord identified and isolated
- External spermatic fascia opened
- Vein identification and ligation (minutes 15-50):
- Each vein carefully dissected and identified
- Typically 8-15 veins requiring ligation
- Testicular artery and lymphatics preserved using Doppler
- Dilated veins double-ligated with fine sutures or clips
- Closure (minutes 50-60):
- Fascia layers closed with absorbable sutures
- Skin closed with subcuticular stitches
- Sterile dressing applied
Immediate Post-Operative Period
Recovery room (1-2 hours):
- Monitoring of vital signs
- Pain medication administered
- Ice pack applied to reduce swelling
- Clear liquids offered once fully awake
Discharge criteria:
- Stable vital signs
- Adequate pain control with oral medications
- Ability to urinate
- Toleration of food/fluids
- Responsible adult present for transportation
Going home:
- Written discharge instructions provided
- Prescription medications given
- Follow-up appointment scheduled (typically 7-14 days)
- 24-hour emergency contact number provided
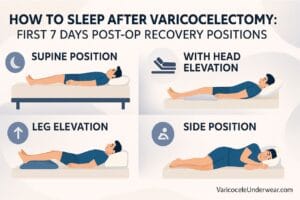
What Recovery Looks Like
The recovery experience varies by surgical approach, but here’s what most patients can expect following microsurgical varicocelectomy.
Post-Operative Recovery: Timeline and Expectations
First 24-48 Hours
Common experiences:
- Mild to moderate groin and scrotal discomfort
- Bruising and swelling around incision site
- Scrotal edema (normal and expected)
- Fatigue from anesthesia
Recovery strategies:
- Apply ice packs for 20 minutes every 2-3 hours
- Take prescribed pain medications on schedule
- Wear supportive underwear 24/7
- Rest with legs elevated
- Avoid standing for prolonged periods
Warning signs requiring immediate attention:
- Severe pain uncontrolled by medication
- Fever above 101°F (38.3°C)
- Excessive bleeding or drainage from incision
- Increasing redness or warmth around wound
- Inability to urinate
Days 3-7
Expected progress:
- Pain decreasing significantly
- Transition from prescription to over-the-counter pain relief
- Bruising may appear worse before improving (normal)
- Incision should remain dry and clean
Activity guidelines:
- Light walking encouraged (promotes circulation)
- No lifting over 10 pounds
- No strenuous exercise or sports
- May shower (pat incision dry afterward)
- No submersion in water (baths, pools, hot tubs)
Return to work:
- Desk jobs: 3-5 days post-surgery
- Moderate physical labor: 1-2 weeks
- Heavy manual labor: 2-3 weeks
Weeks 2-4
Milestones:
- Most men feel back to normal by week 2
- Incision healing well with minimal tenderness
- Scrotal swelling resolving
- Bruising fading to yellow/green discoloration
Activity progression:
- Week 2: Light exercise (walking, stretching, light cycling)
- Week 3: Moderate exercise (jogging, swimming, light weights)
- Week 4: Full return to unrestricted activity including heavy lifting
Sexual activity:
- Masturbation: Safe after 1 week
- Sexual intercourse: Safe after 2 weeks
- No evidence that earlier resumption causes harm, but may be uncomfortable
Months 1-6: Monitoring Results
Semen analysis timeline:
The American Urological Association recommends following this schedule:
- 3 months post-surgery: First semen analysis
- 6 months post-surgery: Second semen analysis
- Maximum improvement typically seen at 3-6 months
- Some men continue improving up to 12 months
Expected improvements:
Research compiled from multiple studies shows:
- Sperm concentration: Average increase of 10-12 million/mL
- Motility: Average improvement of 9-10%
- Morphology: Modest improvement of 1-3%
- DNA fragmentation: Significant decrease in sperm DNA damage
Patient success story: A 29-year-old patient with oligospermia (8 million/mL) underwent microsurgical repair. His pre-operative motility was 25%, and morphology was 2% normal forms. At 3 months post-surgery, concentration improved to 18 million/mL with 35% motility. By 6 months, he reached 28 million/mL with 42% motility, and his partner conceived naturally at 8 months post-procedure.
Long-Term Outcomes
Fertility success rates:
Meta-analysis data published in Fertility and Sterility reports:
- Natural pregnancy rate: 40-50% within 12-18 months
- Live birth rate: 35-40% following varicocele repair
- Success factors: Female age, baseline sperm parameters, varicocele grade
Pain relief outcomes:
- 70-90% of men experience significant or complete pain resolution
- Most improvement occurs within 2-3 months
- Residual discomfort in 5-10% of cases
Testosterone impact:
- Average increase of 80-120 ng/dL
- Most beneficial in men with baseline testosterone <400 ng/dL
- Improvement typically seen within 3-6 months
Potential Complications and How to Minimize Risk
While varicocele surgery is generally safe, understanding potential complications helps you recognize problems early and make informed decisions.
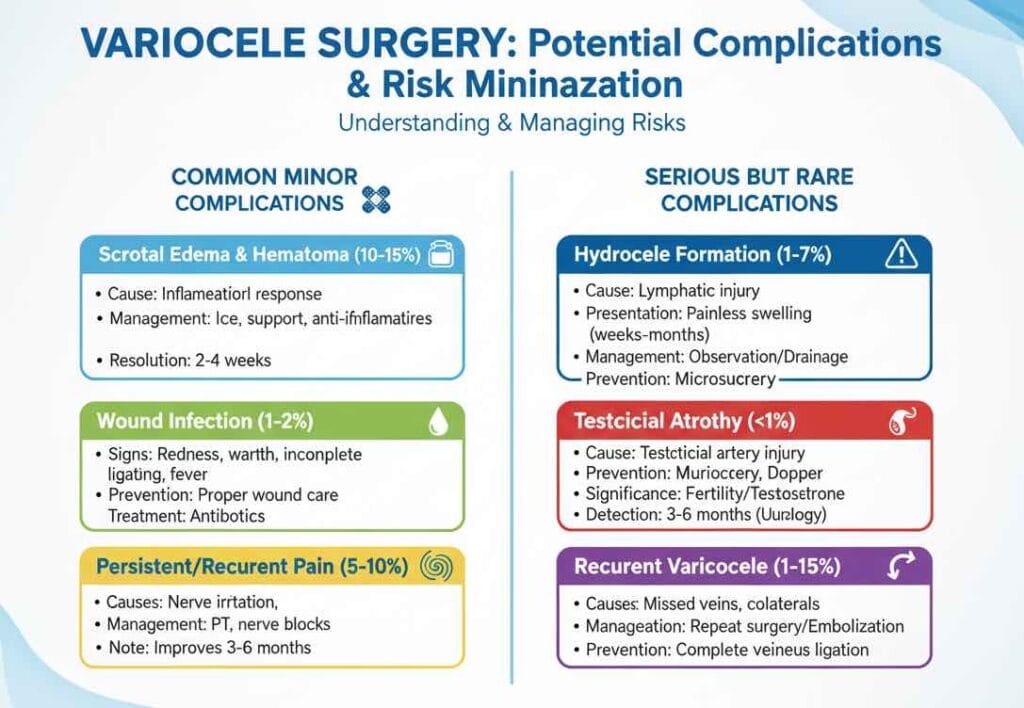
Common Minor Complications
Scrotal edema and hematoma (10-15% of cases):
- Cause: Normal inflammatory response to surgery
- Management: Ice application, supportive underwear, anti-inflammatories
- Resolution: Usually resolves within 2-4 weeks
Wound infection (1-2% of cases):
- Signs: Increasing redness, warmth, purulent drainage, fever
- Prevention: Proper wound care, avoiding submersion
- Treatment: Oral antibiotics; rarely requires wound drainage
Persistent or recurrent pain (5-10% of cases):
- Causes: Nerve irritation, incomplete ligation, unrelated pathology
- Management: Physical therapy, nerve blocks, pain management consultation
- Note: Usually improves over 3-6 months
Serious but Rare Complications
Hydrocele formation (1-7%, depending on technique):
- Cause: Lymphatic vessel injury disrupting fluid drainage
- Presentation: Painless scrotal swelling developing weeks to months post-surgery
- Management: Observation if small; surgical drainage (hydrocelectomy) if large or symptomatic
- Prevention: Microsurgical approach with lymphatic preservation minimizes risk
Testicular atrophy (<1% of cases):
- Cause: Testicular artery injury compromising blood supply
- Prevention: Microsurgical visualization and preservation of artery; intraoperative Doppler use
- Significance: Serious complication that can impact fertility and testosterone
- Detection: Usually evident within 3-6 months; requires urological evaluation
Recurrent varicocele (1-15%, depending on technique):
- Causes: Missed veins during initial surgery, development of collateral vessels
- Presentation: Return of symptoms or physical findings
- Management: May require repeat surgery or embolization
- Prevention: Microsurgical approach with complete venous ligation
Risk Minimization Strategies
Patient factors:
- Smoking cessation 4 weeks before surgery (improves wound healing)
- Optimal diabetes control (HbA1c <7%)
- Maintain healthy weight (reduces surgical complications)
- Disclose all medications and supplements to surgeon
Surgical factors:
- Choose experienced surgeon with specialized training
- Microsurgical technique preferred when available
- Use of surgical Doppler to identify arterial flow
- Complete ligation of all dilated veins
Post-operative care:
- Strict adherence to activity restrictions
- Consistent use of supportive underwear
- Early recognition and reporting of warning signs
- Attendance at all follow-up appointments
Alternative and Complementary Approaches
While surgery remains the definitive treatment for clinically significant varicoceles, several complementary strategies may support recovery and optimize outcomes.
Nutritional Optimization for Sperm Health
Research in Human Reproduction Update identifies key nutrients that support spermatogenesis:
Antioxidant protocol:
- Coenzyme Q10: 200-300mg daily (improves mitochondrial function)
- Vitamin E: 400 IU daily (reduces lipid peroxidation)
- Vitamin C: 500-1000mg daily (water-soluble antioxidant)
- Selenium: 200mcg daily (supports antioxidant enzymes)
- Zinc: 15-30mg daily (essential for sperm production)
- Folic acid: 400-800mcg daily (supports DNA synthesis)
Dietary recommendations:
- Mediterranean diet pattern rich in fruits, vegetables, whole grains
- Omega-3 fatty acids from fish, flaxseed, walnuts
- Limit processed foods, trans fats, and excessive sugar
- Adequate protein intake (1.2-1.6g per kg body weight)
Lifestyle Modifications
Temperature management:
- Avoid hot baths, saunas, and hot tubs
- Limit laptop use on lap (scrotal temperature elevation)
- Choose loose-fitting underwear and pants
- Consider cooling techniques during sleep
Toxin avoidance:
- Minimize alcohol consumption (<14 drinks per week)
- Complete smoking cessation
- Reduce pesticide and BPA exposure
- Avoid excessive use of plastic food containers
Exercise optimization:
- Moderate cardiovascular exercise (150 minutes weekly)
- Resistance training (2-3 sessions weekly)
- Avoid excessive cycling (pressure on scrotum)
- No anabolic steroids or performance-enhancing drugs
Stress Reduction and Mental Health
Studies demonstrate that chronic psychological stress negatively impacts sperm parameters through hormonal pathways:
Evidence-based strategies:
- Mindfulness meditation (10-20 minutes daily)
- Cognitive behavioral therapy for anxiety
- Adequate sleep (7-9 hours nightly)
- Social support and open communication with partner
Integrative Medicine Approaches
Acupuncture:
- Limited evidence suggests potential benefit for sperm parameters
- May help with pain management post-surgery
- Choose licensed, experienced practitioners
Herbal supplements:
- Caution required: Many supplements lack quality control
- Ashwagandha, Tribulus terrestris, and maca have preliminary evidence
- Always discuss with your physician before starting
- Potential interactions with medications
Important note: No complementary approach replaces definitive treatment when clinically indicated. These strategies work best as adjuncts to medical management.
Fertility Outcomes: What the Data Really Shows
For men seeking treatment primarily for fertility reasons, understanding realistic expectations is crucial for decision-making and emotional preparation.
Semen Parameter Improvements
Pre- vs. Post-Surgery Comparisons:
A comprehensive meta-analysis in Asian Journal of Andrology pooling data from 17 studies with 1,241 men found:
| Parameter | Pre-Surgery | Post-Surgery | Mean Improvement |
|---|---|---|---|
| Concentration (million/mL) | 15.4 | 25.2 | +9.8 (64% increase) |
| Motility (%) | 31.2 | 40.6 | +9.4 (30% increase) |
| Morphology (% normal) | 9.8 | 12.2 | +2.4 (24% increase) |
| Total motile count (million) | 18.7 | 38.9 | +20.2 (108% increase) |
Interpretation: While these improvements are statistically significant, not all men achieve pregnancy-level parameters. Approximately 30-40% of men continue to have suboptimal semen quality despite improvement.
Pregnancy Rates: Realistic Expectations
Natural conception outcomes:
Data from The Journal of Urology tracking couples for 24 months post-surgery:
- 6 months: 15-20% pregnancy rate
- 12 months: 30-40% pregnancy rate
- 24 months: 40-50% pregnancy rate
Factors predicting success:
- Female partner age (<35 years significantly better)
- Pre-operative total motile sperm count (>5 million favorable)
- Baseline testicular volume (normal size better prognosis)
- Duration of infertility (<3 years more favorable)
Comparison: Surgery vs. Assisted Reproductive Technology
Cost-benefit analysis:
| Approach | Cost per Cycle | Success per Cycle | Time to Pregnancy |
|---|---|---|---|
| Varicocele repair | $3,000-8,000 (one-time) | 40-50% (24 months) | 6-18 months |
| IUI (Intrauterine insemination) | $500-1,500 | 10-20% | Multiple cycles needed |
| IVF (In vitro fertilization) | $12,000-17,000 | 30-40% | 3-6 months |
| ICSI (IVF with sperm injection) | $15,000-20,000 | 40-50% | 3-6 months |
Decision factors:
- Age and fertility status of female partner
- Severity of male factor infertility
- Financial considerations and insurance coverage
- Time sensitivity for conception
- Patient preference and values
Combined approach: Research suggests that men who undergovaricocelectomy before assisted reproductive technology have improved outcomes with ART procedures:
- Higher fertilization rates during IVF/ICSI
- Better embryo quality
- Increased live birth rates
- Potential to “downgrade” from ICSI to conventional IVF
Clinical case: A 35-year-old patient with severe oligoasthenospermia (5 million/mL, 15% motility) and his 32-year-old partner initially considered proceeding directly to ICSI. After counseling, they opted for microsurgical repair first. Six months post-surgery, parameters improved to 22 million/mL with 38% motility. The couple conceived naturally at 11 months, avoiding the need for ART entirely and saving approximately $15,000-20,000.
When Varicocele Repair Isn’t Enough
Proceeding to ART after surgery:
For couples who don’t achieve pregnancy within 12-18 months post-repair despite improved semen parameters:
- Consider fertility evaluation of female partner
- Reassess semen analysis for stability of improvements
- Discuss timeline preferences and emotional readiness
- Explore IUI as intermediate option if parameters allow
- Consider IVF/ICSI for severe persistent male factor
Salvage options for surgical failure:
- Sperm DNA fragmentation testing (may reveal hidden issues)
- Advanced sperm selection techniques (PICSI, IMSI)
- Testicular sperm extraction (TESE) if ejaculated sperm quality poor
- Consideration of donor sperm in severe cases
Special Populations: Tailored Treatment Considerations
Adolescents and Young Men
Varicocele management in adolescents requires unique considerations given ongoing testicular development.
Current guidelines from the American Academy of Pediatrics:
Indications for intervention:
- Testicular asymmetry >20% or >2mL absolute difference
- Progressive decrease in testicular volume on serial exams
- Abnormal semen analysis in post-pubertal adolescents
- Symptomatic pain affecting quality of life
Observation appropriate when:
- No testicular asymmetry present
- Stable testicular volumes over time
- Grade 1 varicoceles without symptoms
Surgical considerations:
- Microsurgical approach preferred (lowest recurrence)
- Optimal timing: Before completion of puberty for maximum benefit
- Anesthesia: General anesthesia typically used
- Same-day discharge in most cases
Long-term outcomes: Research in The Journal of Urology following adolescents into adulthood found:
- 80% achieved catch-up growth of affected testicle
- Normal semen parameters in 70% at adult follow-up
- Natural conception rates similar to age-matched controls
- Early intervention associated with better outcomes
Parental guidance: I counsel parents that while not all adolescent varicoceles require treatment, documented testicular asymmetry represents a clear indication. The potential future fertility benefits outweigh the minimal surgical risks when performed by experienced surgeons.
Men with Recurrent Varicoceles
Approximately 5-15% of men experience varicocele recurrence, depending on the initial surgical technique used.
Causes of recurrence:
- Missed veins during initial surgery (most common)
- Development of collateral venous pathways
- Incomplete high ligation in retroperitoneal approaches
- Technical failure or inadequate initial repair
Diagnosis:
- Physical examination showing return of varicocele
- Doppler ultrasound confirming venous reflux
- Comparison with pre-operative and post-operative imaging
Management options:
- Repeat microsurgical repair:
- Success rate: 85-95%
- Allows direct visualization of missed vessels
- Lower complication rate than initial surgery
- Preferred for men with fertility concerns
- Percutaneous embolization:
- Excellent option for recurrence after surgery
- Avoids scar tissue from previous operation
- Success rate: 80-90%
- Can address multiple venous pathways
- Observation:
- Appropriate if asymptomatic and fertility goals met
- Regular monitoring for progression
Patient experience: A 38-year-old patient underwent open inguinal varicocelectomy at an outside facility. Eighteen months later, his varicocele returned with worsening pain. Repeat microsurgical subinguinal repair identified three additional dilated veins missed during the initial surgery. Post-operatively, his pain resolved completely, and his previously declining testosterone level improved from 285 ng/dL to 425 ng/dL.
Men with Bilateral Varicoceles
While left-sided varicoceles are most common, approximately 15-20% of men have bilateral disease.
Clinical significance:
- Greater impact on fertility compared to unilateral disease
- More pronounced testosterone deficiency
- Higher likelihood of testicular atrophy
Treatment approach:
- Laparoscopic repair: Allows simultaneous bilateral treatment
- Microsurgical repair: Can be performed bilaterally (longer operative time)
- Embolization: Excellent choice for bilateral cases (single session)
Outcomes:
- Semen improvements comparable to unilateral repair
- Pregnancy rates: 35-45% within 18 months
- Complication rates not significantly higher than unilateral
Older Men and Testosterone Concerns
Emerging research suggests varicoceles may impact testosterone production, making treatment relevant even for men beyond reproductive years.
Evaluation:
- Morning serum total and free testosterone
- Symptoms of hypogonadism (low libido, fatigue, erectile dysfunction)
- Physical examination confirming palpable varicocele
Treatment candidacy:
- Symptomatic hypogonadism (testosterone <300 ng/dL)
- Grade 2-3 varicocele present
- Preference to avoid lifelong testosterone replacement
Expected outcomes:
- Average testosterone increase: 80-120 ng/dL
- 50-60% of men achieve symptomatic improvement
- Effect typically seen within 3-6 months
- May delay or reduce need for testosterone therapy
Important caveat: Varicocele repair should not replace testosterone replacement therapy in men with severe hypogonadism or non-varicocele-related causes. It may serve as an adjunct or allow dose reduction in select cases.
Cost Considerations and Insurance Coverage
Understanding the financial aspects of varicocele treatment helps with planning and reduces surprises.
Average Treatment Costs (United States, 2026)
Surgical procedures (total costs including facility, surgeon, anesthesia):
| Procedure | Without Insurance | With Insurance (After Deductible) |
|---|---|---|
| Microsurgical varicocelectomy | $6,000-12,000 | $1,500-3,500 |
| Laparoscopic varicocelectomy | $8,000-15,000 | $2,000-4,500 |
| Open inguinal repair | $4,000-8,000 | $1,000-2,500 |
| Percutaneous embolization | $5,000-10,000 | $1,500-3,000 |
Additional costs:
- Pre-operative semen analysis: $150-300 per test
- Scrotal ultrasound: $300-600
- Follow-up visits: $150-250 per visit
- Post-operative semen analyses: $150-300 each (typically 2-3 needed)
Insurance Coverage Guidelines
Medical necessity criteria (typical insurance requirements):
Most insurance plans cover varicocele repair when:
- Documented abnormal semen parameters AND couple infertility
- Clinically palpable varicocele (grade 2 or 3)
- Conservative management attempted for 3-6 months
- No female factor as sole cause of infertility
OR
- Symptomatic pain unresponsive to conservative treatment
- Testicular atrophy with documented size discrepancy
Pre-authorization:
- Required by most insurance plans
- Typically takes 5-10 business days
- Documentation needed: physical exam findings, ultrasound, semen analyses
- Prior authorization denial can be appealed with supporting evidence
Coverage challenges:
- Some plans exclude fertility-related procedures
- “Cosmetic” concerns typically not covered
- Testosterone improvement alone may not meet criteria
- Out-of-network providers may require higher out-of-pocket costs
Financial assistance options:
- Hospital payment plans (often interest-free for 6-12 months)
- Healthcare credit cards (CareCredit, similar programs)
- Health Savings Accounts (HSA) or Flexible Spending Accounts (FSA)
- Negotiated cash-pay discounts at some facilities
Cost-Effectiveness Analysis
Health economics research comparing varicocele repair to proceeding directly to IVF/ICSI:
Cost per live birth:
- Varicocele repair followed by natural conception attempts: $6,000-15,000
- IVF/ICSI (average 2-3 cycles needed): $30,000-60,000
Conclusion: For couples with isolated male factor infertility and no severe female factors, varicocele repair is cost-effective as first-line treatment, particularly when female partner is under age 35.
Maximizing Your Recovery: Expert Tips
Drawing from clinical experience and patient feedback, these strategies optimize healing and outcomes.
Physical Recovery Optimization
Week 1 priorities:
- Ice religiously: 20 minutes on, 40 minutes off during waking hours
- Elevate consistently: Hips higher than chest when lying down
- Support 24/7: Quality supportive underwear makes tremendous difference
- Gentle movement: Short walks every 2-3 hours prevent stiffness
- Stay ahead of pain: Take medications on schedule, not as-needed
Weeks 2-4 strategies:
- Gradual progression: Increase activity by 10-20% weekly
- Listen to your body: Some discomfort normal; sharp pain means slow down
- Compression continues: Wear support during all physical activity
- Scar massage: Gentle circular massage after 2 weeks promotes healing
- Hydration: 8-10 glasses water daily supports tissue repair
Nutritional Support for Healing
Anti-inflammatory diet (first 2-4 weeks):
- Fatty fish rich in omega-3s (salmon, sardines, mackerel)
- Colorful vegetables and berries (high antioxidant content)
- Turmeric with black pepper (enhances absorption)
- Ginger tea (natural anti-inflammatory)
- Avoid: processed foods, excessive sugar, alcohol
Protein optimization:
- Target: 1.2-1.6g protein per kg body weight
- Distribute across meals for optimal synthesis
- Include: lean meats, eggs, Greek yogurt, legumes
- Consider protein shake if appetite reduced
Fertility Optimization Post-Surgery
Timeline strategy:
- Months 1-3: Focus on recovery and lifestyle optimization
- Month 3: First post-operative semen analysis
- Months 3-6: Begin conception attempts if parameters improved
- Month 6: Second semen analysis to confirm sustained improvement
- Months 6-18: Continue natural conception attempts
Conception-boosting behaviors:
- Timing: Intercourse every 2-3 days during fertile window
- Avoid lubricants: Most are sperm-toxic; use Pre-Seed if needed
- Manage heat: No hot baths, laptops on lap, tight underwear
- Supplement continuation: Maintain antioxidant protocol for 6-12 months
- Stress reduction: High cortisol negatively impacts sperm parameters
When to seek help:
- No improvement in semen parameters at 6 months
- No conception after 12 months with improved parameters (if female <35)
- No conception after 6 months with improved parameters (if female >35)
- Worsening parameters despite surgery
Psychological and Relationship Support
Common emotional challenges:
- Anxiety while waiting for semen analysis results
- Disappointment if improvement slower than hoped
- Stress related to conception attempts
- Relationship tension around infertility
Coping strategies:
- Set realistic expectations: Remember 6-12 months for maximum improvement
- Maintain intimacy: Sex isn’t just for conception
- Share feelings: Open communication with partner crucial
- Seek support: Consider fertility counseling if struggling
- Celebrate progress: Acknowledge improvements even if conception hasn’t occurred
Partner involvement:
- Attend follow-up appointments together when possible
- Share responsibility for lifestyle modifications
- Support each other through the emotional journey
- Consider joint fertility evaluation to address all factors
Frequently Asked Questions
How long does it take to see improvement in sperm count after varicocele surgery?
Most men begin seeing improvements in semen parameters around 3 months post-surgery, with maximum benefit typically occurring between 3-6 months. This timeline reflects the 72-day sperm production cycle—sperm analyzed 3 months after surgery began developing shortly after the procedure. Studies show that some men continue to experience improvements up to 12 months post-operatively. I recommend semen analysis at 3 and 6 months to track progress. If you’re not seeing meaningful improvement by 6 months, discuss alternative fertility approaches with your urologist, as approximately 30-40% of men don’t achieve pregnancy-level parameters despite surgery.
Can a varicocele come back after surgery, and what causes recurrence?
Yes, varicoceles can recur in 1-15% of cases depending on the surgical technique used. Recurrence is most commonly caused by missed veins during the initial surgery—there can be 8-15 dilated veins requiring ligation, and incomplete identification leads to continued blood pooling. Other causes include development of new collateral vessels or technical issues with the initial repair. Microsurgical approaches have the lowest recurrence rate (1-2%) because high-powered magnification allows identification of all abnormal veins. If recurrence occurs, repeat microsurgical repair or percutaneous embolization are both effective options with success rates of 85-95%. Regular follow-up with physical examination helps detect recurrence early.
Is varicocele surgery worth it if I’m not trying to have children right now?
The decision depends on your individual circumstances. If you’re experiencing chronic pain that impacts your quality of life, surgery offers a 70-90% chance of significant relief, making it worthwhile regardless of fertility plans. For asymptomatic men with normal semen parameters who aren’t currently pursuing pregnancy, observation is typically appropriate—not all varicoceles require treatment. However, if you have documented testicular atrophy (affected testicle is 20% smaller) or progressive decline in semen parameters, repair can prevent further damage even if you’re delaying parenthood. Research suggests that earlier treatment in young men may preserve long-term fertility potential. Discuss your specific situation, symptoms, and future family plans with a urologist to determine the best timing for intervention.
Conclusion: Making an Informed Decision About Varicocele Treatment
Varicocele treatment in 2026 represents a success story of evidence-based medicine—we have multiple effective options supported by decades of research, clear guidelines for when intervention benefits patients, and excellent outcomes for both fertility and symptom relief when appropriately selected.
Key Takeaways
Treatment is indicated when:
- Documented infertility with abnormal semen parameters
- Chronic pain affecting quality of life
- Testicular atrophy or progressive size discrepancy
- Symptomatic testosterone deficiency with palpable varicocele
Observation is appropriate when:
- Asymptomatic with normal fertility evaluation
- Female factor infertility is the primary concern
- Grade 1 varicocele without complications
- Family planning complete and no symptoms present
Microsurgical varicocelectomy offers:
- Highest success rates (60-70% semen improvement)
- Lowest complication and recurrence rates (1-2%)
- Natural pregnancy in 40-50% of infertile couples
- Pain relief in 70-90% of symptomatic men
- Potential testosterone improvement of 80-120 ng/dL
Recovery expectations:
- 1-2 weeks until return to normal activities
- 3-6 months for maximum semen parameter improvement
- 6-18 months for natural conception attempts
- Minimal complications with proper surgical technique
Your Next Steps
If you’ve been diagnosed with a varicocele or suspect you might have one:
- Schedule evaluation: Physical examination, semen analysis, and scrotal ultrasound establish baseline
- Assess impact: Determine whether your varicocele is affecting fertility, causing pain, or producing testicular atrophy
- Try conservative measures: Supportive underwear, lifestyle modifications, and pain management for 3-6 months
- Consult a specialist: Urologist or reproductive urologist experienced in microsurgical techniques
- Make informed decision: Weigh benefits, risks, costs, and alternatives based on your individual circumstances
- Optimize recovery: Follow post-operative guidelines and lifestyle modifications for best outcomes
Final Thoughts
As a urologist specializing in male fertility and varicocele treatment, I’ve witnessed countless men progress from anxiety and frustration about their diagnosis to successful outcomes—whether that means achieving a long-desired pregnancy, eliminating chronic pain, or simply gaining peace of mind about their reproductive health.
Varicocele treatment isn’t right for everyone, but for men with clear indications, modern surgical techniques offer safe, effective solutions with excellent success rates. The key is individualized care: understanding your specific situation, goals, and concerns, then developing a treatment plan aligned with your values and priorities.
Remember that varicocele repair is one tool in the fertility and men’s health toolkit. Success requires patience—sperm production takes time, and conception depends on multiple factors beyond male parameters alone. Stay engaged with your healthcare team, maintain healthy lifestyle habits, and approach the journey with realistic expectations and hope.
If you’re struggling with symptoms or concerns about fertility, don’t suffer in silence. Reach out to a qualified urologist who can provide expert guidance, compassionate care, and evidence-based treatment tailored to your needs. With the right approach, most men with varicoceles can achieve their health and fertility goals.
Medical Disclaimer: This article provides general educational information about varicocele treatment and should not replace personalized medical advice. Every patient’s situation is unique. Consult with a qualified urologist or healthcare provider for evaluation and treatment recommendations specific to your circumstances. Treatment outcomes vary based on individual factors, and no specific results can be guaranteed.