Testicular shrinkage from varicocele raises serious concerns about fertility and long-term reproductive health. Research shows that 60-80% of young patients experience partial or complete testicular volume recovery after surgical treatment, but outcomes depend heavily on timing, age, and severity of the condition. Understanding whether your testicular atrophy can be reversed requires examining multiple factors that influence tissue regeneration and treatment success.
What Causes Testicular Atrophy in Varicocele Patients
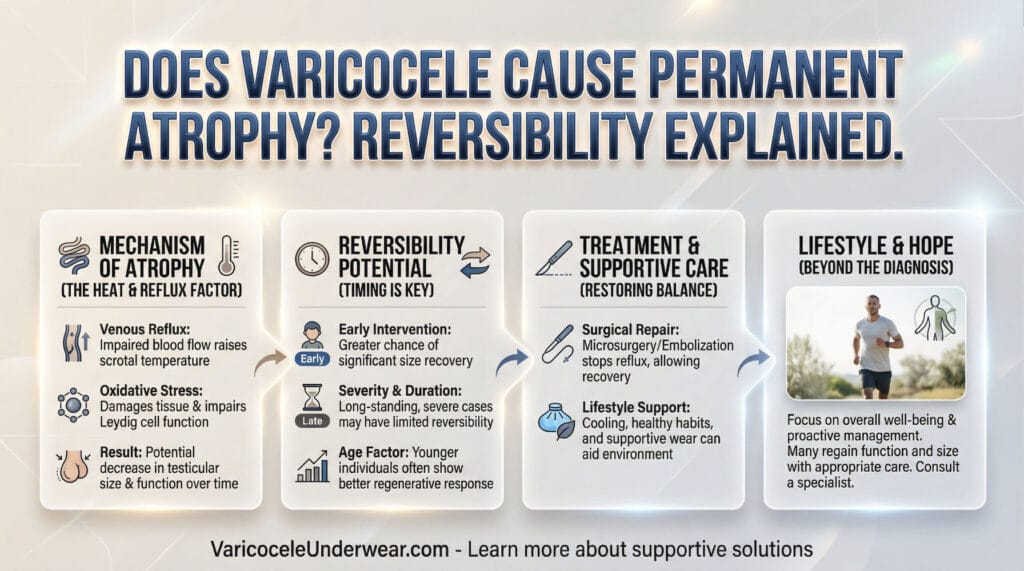
Varicocele occurs when veins in the scrotum become enlarged, creating a complex network of swollen vessels that impair normal blood drainage from the testicle. This abnormal venous pooling increases testicular temperature and creates oxidative stress that gradually damages sperm-producing tissue. The condition affects approximately 15-20% of all adult males but is found in up to 40% of men evaluated for infertility.
The left testicle experiences atrophy more frequently because the left testicular vein connects to the higher-pressure left renal vein, making blood flow problems more likely on this side. When blood pools in these enlarged veins, the testicle receives less oxygen and nutrients while being exposed to higher temperatures and toxic metabolites. Over time, this environment causes the testicular tissue to shrink, reducing both size and function.
Can Testicular Volume Return to Normal After Varicocele Repair
Yes, testicular atrophy from varicocele can be reversed in many cases, particularly when identified and treated early. Studies measuring testicular volume before and after varicocelectomy found that adult patients experienced an average increase of 1.5 mL in the affected testicle and 2.4 mL in total testicular volume. These improvements occurred alongside better sperm counts and motility, demonstrating that structural recovery correlates with functional improvement.
The reversibility depends on several critical factors:
- Patient age at treatment – Adolescents and young adults show the highest recovery rates due to greater tissue regeneration capacity
- Duration of varicocele presence – Long-standing conditions with prolonged atrophy respond less favorably to intervention
- Severity of tissue damage – Mild to moderate atrophy reverses more completely than severe, chronic shrinkage
- Timing of surgical correction – Early intervention offers the best chance of restoring normal testicular size
Recovery Rates by Age Group
Adolescent patients demonstrate the most impressive recovery statistics, with 60-80% experiencing partial or full restoration of testicular size after varicocelectomy. A study tracking young patients found catch-up growth rates of up to 1.37 mL per year following percutaneous varicocele repair. Boys younger than 14 years showed statistically higher increases in testicular volume compared to older adolescents.
Adult men also benefit from surgical correction, though improvement is less predictable than in younger patients. Research tracking adults with clinical left varicocele found that left testicular volume increased significantly by an average of 1.5 mL after repair, accompanied by improvements in sperm concentration and motility percentage.
How Long Does Testicular Recovery Take After Varicocele Surgery
Testicular volume changes develop gradually over months following varicocelectomy. Sperm production requires approximately 74 days to complete one full cycle, meaning noticeable improvements in semen parameters typically appear 3-4 months after surgery. Full testicular recovery and stabilization of volume measurements generally occurs within 6-12 months post-operatively.
Supportive underwear designed for varicocele can provide symptom relief during the recovery period by reducing discomfort and supporting proper scrotal positioning. Specialized varicocele underwear with cooling and support features may help maintain optimal temperature and reduce strain on the affected area as healing progresses.
The timeline for specific improvements includes:
- 2-4 weeks: Reduction in testicular pain and discomfort
- 3-6 months: Measurable improvements in sperm quality and semen volume
- 6-12 months: Full recovery of testicular volume and testosterone production
- Up to 1 year: Final stabilization of all parameters
When Is Testicular Atrophy Permanent and Irreversible
Not all cases of varicocele-induced atrophy can be reversed. Permanent damage occurs when intervention is delayed for years, allowing progressive tissue destruction that exceeds the testicle’s regenerative capacity. Severe atrophy with extensive loss of seminiferous tubules and supporting structures may not respond to surgical correction.
Factors indicating poor reversibility potential:
- Varicocele present for many years without treatment
- Severe testicular shrinkage exceeding 20% size difference between testicles
- Very low baseline sperm counts or absent sperm production
- Advanced patient age with limited tissue regeneration capacity
- Pre-existing hormonal disorders or fertility conditions
When permanent damage has occurred, natural conception may still be possible through assisted reproductive techniques such as intracytoplasmic sperm injection (ICSI), which requires only small numbers of viable sperm.
Treatment Options and Success Rates for Reversing Atrophy
Microsurgical varicocelectomy represents the gold standard treatment for clinically significant varicocele with testicular atrophy. This procedure involves identifying and ligating the enlarged veins while preserving the testicular artery and lymphatic vessels, minimizing complications while maximizing effectiveness.
Treatment success varies by approach:
| Treatment Method | Recurrence Rate | Testicular Volume Improvement | Fertility Improvement |
|---|---|---|---|
| Microsurgical varicocelectomy | <5% | 60-80% of young patients | 40-60% pregnancy rates |
| Laparoscopic repair | ~15% | Moderate improvement | Variable outcomes |
| Percutaneous embolization | ~11% | Similar to surgical approaches | Lower pregnancy rates than surgery |
Meta-analyses examining varicocele repair outcomes found expected improvements of 9.71-12.32 million/mL in sperm count, 10.86% increase in motility, and 9.69% improvement in morphology. Surgical correction of clinically significant varicoceles in infertile males with abnormal semen parameters significantly improves sperm parameters and pregnancy rates.
Patients with initial sperm counts above 8 million/mL and progressive motility exceeding 18% experience the most substantial post-operative improvements.
Monitoring Testicular Health After Varicocele Diagnosis
Regular monitoring allows early detection of progressive atrophy and timely intervention. Physical examination every 6-12 months helps track testicular size, consistency, and varicocele progression. Ultrasound imaging provides objective volume measurements and identifies subclinical changes not detectable by palpation.
For men with fertility concerns, semen analysis should be performed before treatment and repeated 4 months post-operatively to assess response. Hormone testing including testosterone and follicle-stimulating hormone levels provides additional data about testicular function and recovery potential.
Boys and adolescents with a testicular size difference exceeding 20% between sides should be considered for early surgical correction to prevent future infertility and maximize the potential for catch-up growth. Early intervention in this age group offers the best opportunity for complete reversal of atrophy.
FAQ
Q: Will my testicle return to normal size after varicocele surgery?
Recovery depends on your age and how long atrophy has been present. Adolescents and young men have 60-80% chance of significant volume restoration, while adults typically experience 1.5-2.4 mL increases. Early treatment within the first few years of atrophy offers the best reversal potential. Long-standing severe atrophy may show limited improvement.
Q: How quickly can I expect to see testicular size improvement after varicocelectomy?
Testicular volume changes occur gradually over 6-12 months following surgery. Initial improvements in blood flow happen immediately, but tissue regeneration requires time. Most patients notice measurable size increases by 3-4 months, with full recovery stabilizing around 6-12 months post-operatively. Younger patients generally experience faster and more complete recovery.
Q: Can I prevent testicular atrophy if I already have varicocele?
Early surgical correction prevents progressive atrophy in most cases. If you have a clinically significant varicocele with testicular size difference, abnormal semen parameters, or declining fertility, prompt treatment minimizes long-term damage. Regular monitoring with physical exams and ultrasound helps identify worsening atrophy before it becomes irreversible. Delaying treatment increases the risk of permanent tissue loss.