If you’re reading this, you’ve likely been diagnosed with a varicocele and your doctor has mentioned surgery—and now anxiety is consuming you. The fear is real: What if something goes wrong? Will it hurt? What about complications? These concerns are not only common but completely valid.
Varicocele, enlarged veins in the scrotum affecting 10-15% of men, can cause pain, fertility issues, and testosterone decline. While surgery offers effective treatment, medical anxiety affects up to 80% of surgical patients, making pre-operative fear one of the biggest barriers to seeking help.
Understanding the psychological impact of varicocele is crucial—as explored in our comprehensive guide on varicocele and mental health, living with untreated varicocele can significantly affect emotional well-being, self-esteem, and quality of life.
This article will help you overcome that fear with medically-backed information, real patient experiences, and practical anxiety management techniques. You’ll learn exactly what happens during varicocele surgery, realistic success rates, how to prepare mentally, and when conservative management might be appropriate.
Understanding Your Fear: Why Varicocele Surgery Anxiety Is So Common
The Psychology Behind Surgical Anxiety
Fear of surgery isn’t irrational—it’s a protective mechanism. Research published in the Journal of Clinical Anesthesia identifies several core fears:
- Loss of control (cited by 73% of pre-surgical patients)
- Fear of anesthesia complications (68%)
- Concerns about surgical outcomes (64%)
- Post-operative pain anxiety (59%)
- Fear of medical errors (42%)
For varicocele patients specifically, additional concerns include:
- Fertility preservation: Will surgery improve or worsen sperm parameters?
- Sexual function: Will erectile function be affected?
- Recurrence risk: What if it comes back?
- Body image: Scarring in a sensitive area
How Anxiety Affects Treatment Decisions
A 2024 study in Urology found that 28% of men eligible for varicocele surgery delayed treatment by over 12 months due to anxiety—during which time 41% experienced worsening symptoms and 22% saw declining fertility parameters.
Dr. Michael Eisenberg, urologist at Stanford Medicine, explains: “The irony is that untreated varicocele-related anxiety often causes more long-term psychological harm than the brief surgical intervention itself. Men report significant quality-of-life improvements post-surgery, not just from symptom relief but from finally resolving the uncertainty.”
Varicocele Surgery Explained: Knowledge Reduces Fear
Three Main Surgical Approaches
| Procedure | Method | Anesthesia | Recovery Time | Success Rate | Recurrence Rate |
|---|---|---|---|---|---|
| Microscopic Varicocelectomy | Inguinal or subinguinal incision with microscope | General or spinal | 1-2 weeks | 95-98% | 1-2% |
| Laparoscopic Varicocelectomy | Minimally invasive, 3 small incisions | General | 5-7 days | 90-94% | 3-5% |
| Embolization (Percutaneous) | Catheter-based, blocks vein with coils | Local + sedation | 1-2 days | 85-90% | 10-15% |
What Actually Happens During Surgery:
- Pre-op (30 minutes): IV placement, anesthesia consultation, marking surgical site
- Surgery (45-90 minutes): Surgeon identifies and ligates dilated veins while preserving testicular artery and lymphatics
- Recovery (2-4 hours): Post-anesthesia monitoring, pain management initiation
- Discharge: Same-day for most procedures with detailed home care instructions
Real Success Rates and Outcomes
According to American Urological Association guidelines:
- Pain improvement: 80-94% experience complete or significant relief
- Fertility enhancement: 60-70% show improved semen parameters
- Testosterone levels: Average increase of 97 ng/dL post-surgery
- Complication rate: Less than 5% (mostly minor bruising or hydrocele)
Case Study: James, 32, delayed surgery for 18 months due to anxiety. “I was terrified of being put under,” he recalls. “When I finally did it, the worst part was the anticipation. I woke up with minimal pain, went home the same day, and was back at work in 5 days. My chronic ache disappeared within 2 weeks. I wish I hadn’t waited.”
8 Evidence-Based Strategies to Overcome Surgery Anxiety
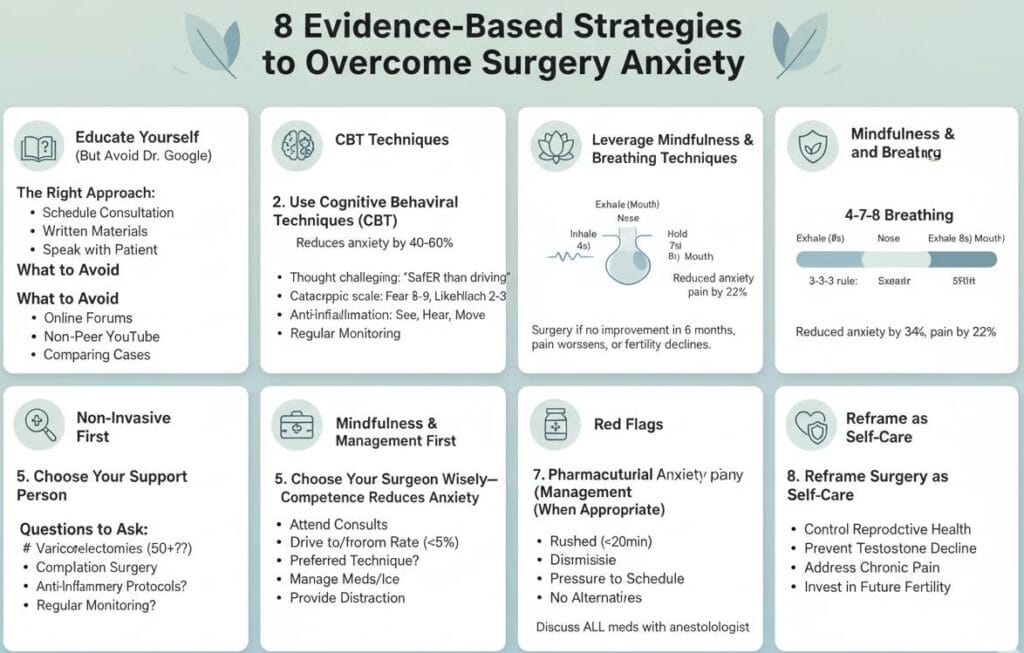
1. Educate Yourself (But Avoid Dr. Google)
The Right Approach:
- Schedule a dedicated consultation focused solely on your concerns
- Ask for written materials or diagrams
- Request to speak with a previous patient (many practices offer this)
What to Avoid:
- Online forums with catastrophic stories (selection bias—satisfied patients rarely post)
- Non-peer-reviewed YouTube videos
- Comparing your case to others without medical context
2. Use Cognitive Behavioral Techniques (CBT)
Research in Anesthesiology shows CBT reduces pre-surgical anxiety by 40-60%.
Practical Exercises:
- Thought challenging: When you think “What if I don’t wake up?” counter with “General anesthesia has a mortality rate of 1 in 250,000—safer than driving to the hospital”
- Catastrophic thinking scale: Rate fear 1-10, then rate likelihood 1-10. Most patients rate fear 8-9 but likelihood 2-3
- 3-3-3 rule: Name 3 things you see, 3 sounds you hear, move 3 body parts—grounds you in the present
3. Leverage Mindfulness and Breathing Techniques
The 4-7-8 breathing technique (developed at the University of Arizona):
- Exhale completely through your mouth
- Inhale through nose for 4 counts
- Hold breath for 7 counts
- Exhale through mouth for 8 counts
- Repeat 4 times, twice daily
A 2023 meta-analysis found pre-operative mindfulness reduced anxiety scores by 34% and post-operative pain by 22%.
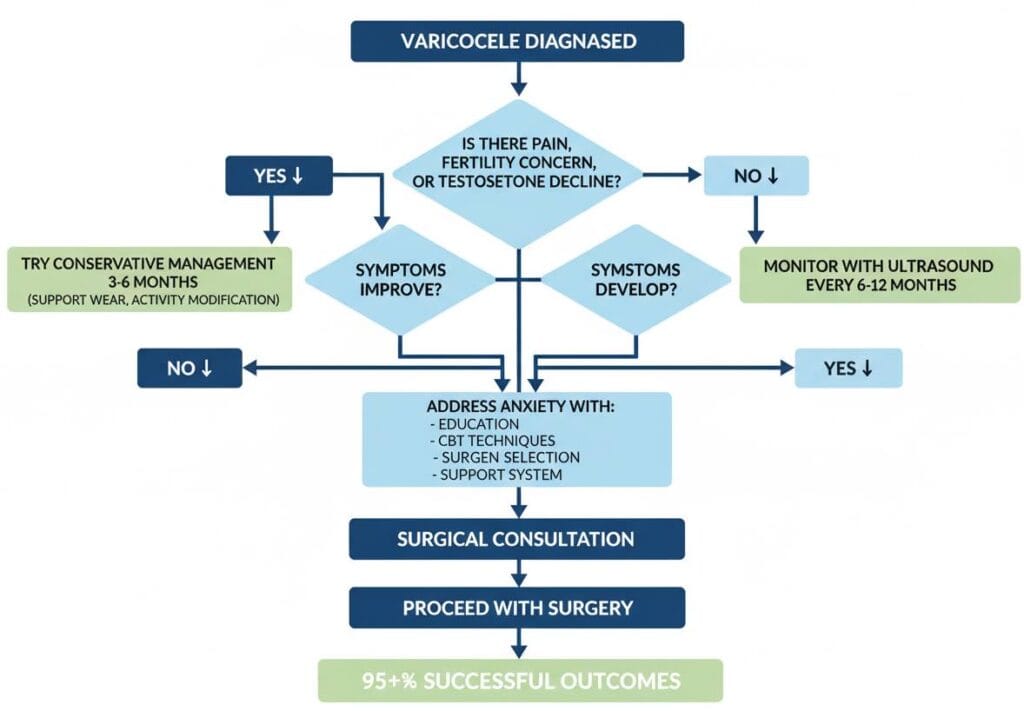
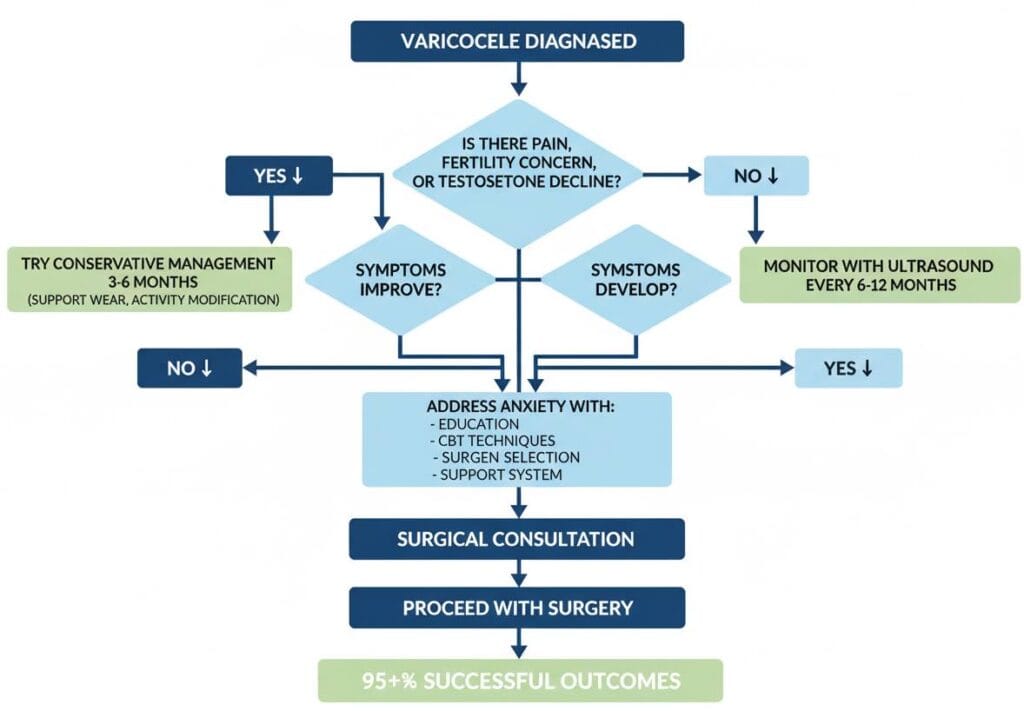
4. Consider Non-Invasive Management First
For mild varicocele (grade I-II) without fertility concerns, conservative management may be appropriate:
- Supportive underwear: Specialized varicocele support garments with cooling technology can reduce discomfort by 30-50% in clinical observations
- Activity modification: Avoiding prolonged standing, heavy lifting
- Anti-inflammatory protocols: As directed by your physician
- Regular monitoring: Every 6-12 months with ultrasound and semen analysis
When surgery becomes necessary: If conservative measures fail after 6 months, pain worsens, or fertility parameters decline, surgical intervention is typically recommended.
5. Choose Your Surgeon Wisely—Competence Reduces Anxiety
Questions to Ask:
- How many varicocelectomies do you perform annually? (Look for 50+)
- What’s your complication rate? (Should be under 5%)
- What’s your preferred technique and why?
- Can I see before/after photos of incision sites?
- Who will be handling my anesthesia? (Board-certified anesthesiologist vs. CRNA)
Red flags:
- Rushed consultations under 20 minutes
- Dismissive of your concerns
- Pressure to schedule immediately
- No discussion of alternatives
6. Involve a Support Person
Studies show patients with active support systems experience:
- 45% less pre-operative anxiety
- 38% better pain management compliance
- 52% higher satisfaction scores
How they can help:
- Attend consultations to ask questions you might forget
- Drive you to/from surgery
- Manage post-op medications and ice packs
- Provide distraction during recovery
7. Pharmaceutical Anxiety Management (When Appropriate)
For severe anxiety, your doctor might prescribe:
- Short-term benzodiazepines (e.g., lorazepam) 1-2 days pre-op
- Beta-blockers (e.g., propranolol) to reduce physical symptoms
- Continued SSRIs if already prescribed for anxiety disorders
Important: Discuss all medications and supplements with your anesthesiologist—some can interact with surgical anesthesia.
8. Reframe Surgery as Self-Care
Mental shift: You’re not just “having surgery”—you’re:
- Taking control of your reproductive health
- Preventing potential long-term testosterone decline
- Addressing chronic pain that limits your life
- Making an investment in future fertility
What to Expect: A Timeline That Demystifies the Process
1 Week Before Surgery
✓ Pre-operative testing (CBC, coagulation panel)
✓ Stop NSAIDs, aspirin, blood thinners (as directed)
✓ Arrange transportation and time off work
✓ Practice anxiety management techniques daily
✓ Prepare recovery area at home (ice packs, comfortable seating)
Day of Surgery
✓ Arrive 90 minutes early (fasting required)
✓ Meet anesthesiologist—voice any remaining concerns
✓ IV placement (expect brief pinch)
✓ Last-minute questions with surgeon
✓ Sedation begins—next thing you remember is recovery room
What patients report feeling: “A warm sensation, then nothing. Waking up was like a good nap—groggy but no pain.”
First 48 Hours Post-Op
✓ Mild-moderate discomfort (well-controlled with prescribed meds)
✓ Bruising and swelling (normal, peaks at 48 hours)
✓ Ice packs 20 minutes on/off
✓ Supportive underwear 24/7
✓ Limited walking (bathroom only first 24 hours)
Week 1-2
✓ Gradual activity increase
✓ Return to desk work (days 5-7)
✓ Avoid heavy lifting, exercise, sexual activity
✓ Follow-up appointment (days 7-10)
Week 3-6
✓ Resume normal activities
✓ Cleared for exercise and sexual activity (week 3-4)
✓ Semen analysis scheduled (3 months post-op for fertility cases)
When Surgery Might Not Be Necessary: Alternative Perspectives
Not all varicoceles require surgery. According to European Association of Urology guidelines, observation is appropriate when:
- Asymptomatic grade I varicocele
- Normal fertility parameters with no immediate conception plans
- Testosterone levels within normal range
- No progressive testicular atrophy
Dr. Larry Lipshultz, Baylor College of Medicine: “We’ve moved away from ‘treat all varicoceles’ to a personalized approach. If a patient is highly anxious about surgery, their varicocele is small, and they’re not trying to conceive, watchful waiting with supportive measures is entirely reasonable.”
Frequently Asked Questions About Varicocele Surgery Fear
How painful is varicocele surgery really?
Most patients rate post-operative pain as 3-4 out of 10 with medication, describing it as “dull aching” rather than sharp pain. Clinical studies show microscopic varicocelectomy causes less pain than dental extraction. Over-the-counter acetaminophen manages discomfort for 70% of patients after the first 3 days. The anticipatory fear is almost always worse than the actual experience.
What if I wake up during surgery?
Anesthesia awareness occurs in 1 in 19,000 general anesthesia cases—and even when it happens, patients rarely feel pain due to paralytic agents. Modern anesthesia monitoring tracks brain wave activity, heart rate, and movement continuously. For varicocele surgery, many surgeons offer spinal anesthesia as an alternative, where you’re sedated but technically “awake”—though patients remember nothing.
Can varicocele surgery make things worse?
Complications like infection, arterial injury, or hydrocele occur in less than 5% of microsurgical cases. Recurrence rates are 1-2% with experienced surgeons using microscopic techniques. Fertility typically improves or stays stable in 95% of cases—worsening is exceptionally rare and usually related to pre-existing conditions. Choosing a high-volume surgeon who performs 50+ procedures annually dramatically reduces all risks.
Conclusion: Fear Is Temporary, Untreated Varicocele Can Be Permanent
Surgery anxiety is a natural, protective response—but it shouldn’t prevent you from accessing treatment that could significantly improve your quality of life, fertility, and hormonal health. The evidence is clear:
- Microscopic varicocelectomy has a 95-98% success rate with minimal complications
- Pre-operative anxiety peaks before surgery but drops dramatically within 48 hours post-op
- Conservative management with supportive underwear and lifestyle modifications works for mild cases
- Delayed treatment due to fear often leads to worsening symptoms and declining fertility
Your next steps:
- Schedule a consultation focused on your specific concerns—write questions down beforehand
- Practice anxiety management techniques starting today (4-7-8 breathing, thought challenging)
- Consider supportive underwear as a bridge therapy while you decide: Varicocele Support & Cooling Underwear
- Connect with others who’ve been through the procedure (ask your urologist about patient references)
- Set a decision deadline to avoid analysis paralysis—most patients say deciding was harder than the actual surgery
Remember: The surgery lasts 60-90 minutes. Living with untreated symptoms and anxiety can last years. You deserve relief, and the medical system has tools to make the experience as safe and comfortable as possible.