Varicocele pain isn’t one-size-fits-all. The type of discomfort you feel—whether it’s a dull ache or sharp stabbing—gives doctors important clues about your condition and how well treatment might work. About 2% to 10% of men with varicocele experience pain, and understanding your pain pattern is the first step to finding relief.
This guide breaks down what different pain types mean, when they signal something serious, and which symptoms respond best to treatment. For complete background on varicocele conditions, read our comprehensive varicocele guide.
Why Pain Type Matters for Diagnosis
The character of your pain isn’t just about discomfort. It’s diagnostic data.
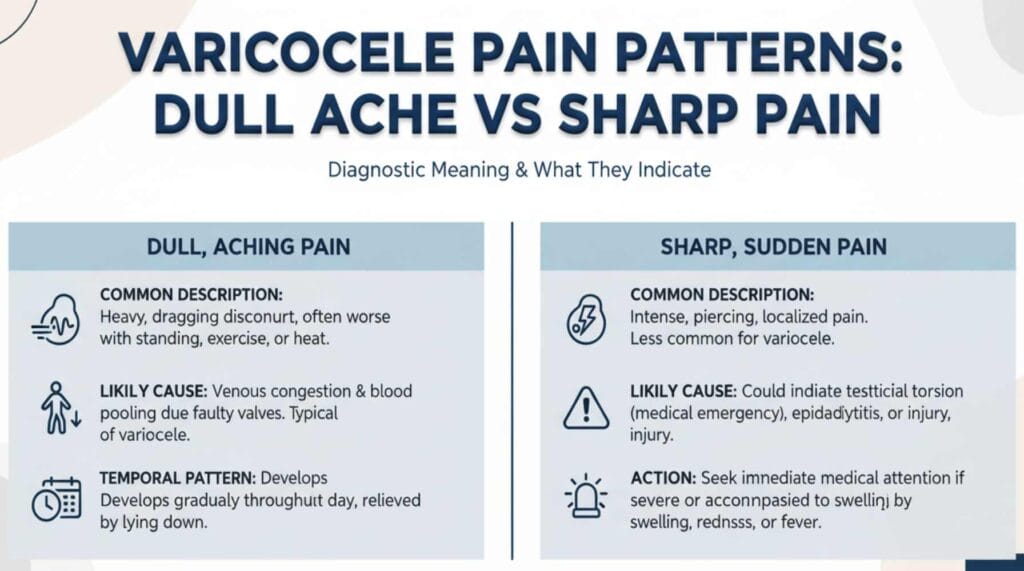
Testicular pain from varicocele typically presents as a dull, aching, or throbbing sensation in the testicle, scrotum, or groin, though some men experience acute, sharp, or stabbing pain. Doctors use pain characteristics to predict treatment success rates. Research shows men who describe their pain as “dull” or “dragging” have a 100% success rate with surgical repair, compared to 78.4% for those reporting “aching” pain.
Why? Dull pain localized to the scrotum that worsens with standing typically indicates classic varicocele mechanics—blood pooling in enlarged veins. Sharp or radiating pain may involve nerve compression or other conditions, making diagnosis more complex.
Dull Ache: Classic Varicocele Pain Pattern
Most men with symptomatic varicocele describe their discomfort as a dull ache or heaviness. This pain has specific patterns:
- Worsens when standing for long periods
- Intensifies during exercise or physical activity
- Improves when lying down
- Feels like a “dragging” sensation in the scrotum
- Gets worse as the day progresses
This pattern happens because gravity causes blood to pool in the enlarged veins of your pampiniform plexus. When you stand, venous pressure increases. When you lie down, blood drains more easily back toward your heart.
The dull ache typically doesn’t come with sudden onset. It develops gradually and becomes noticeable during activities that raise scrotal temperature or increase abdominal pressure. Men often describe it as “background discomfort” rather than acute pain.
What Dull Pain Predicts About Treatment
Dull, aching pain is actually good news for treatment outcomes. Studies tracking surgical repair show that patients with classic dull pain patterns experience complete pain resolution in 86-90% of cases. The predictable nature of this pain suggests straightforward varicocele mechanics without complicated secondary issues.
Sharp Pain: Less Common But Important
While rare, some men with varicocele experience sharp or stabbing pain. This pain type raises different diagnostic questions.
Sharp varicocele pain may indicate:
- Nerve compression from severely enlarged veins
- Rapid changes in venous pressure
- Concurrent conditions like hernias or kidney stones
- Grade 3 (severe) varicocele with massive vein dilation
Sharp pain radiating to the groin or thigh may persist after surgery more often than localized dull pain. This doesn’t mean treatment won’t work, but it signals doctors to investigate additional causes.
Sudden onset sharp pain warrants immediate medical evaluation. While varicocele pain typically develops gradually, acute pain could indicate testicular torsion or other emergencies.
Pain Location Tells a Story
Where you feel pain matters as much as what type.
Scrotum-only pain: Classic varicocele. Pain stays in the scrotal sac, often on the left side (90% of varicoceles are left-sided). This localized pattern suggests the veins themselves are the primary pain source.
Inguinal (groin) pain: Indicates the varicocele extends higher up the spermatic cord. Pain in the inguinal canal area suggests the dilated veins reach beyond the scrotum into the groin region.
Lower abdominal pain: May involve referred pain from increased venous pressure affecting structures beyond the immediate varicocele. Doctors must rule out other abdominal or urological conditions.
Radiating pain to thigh: Less common and requires broader investigation. While still potentially varicocele-related, radiating patterns suggest nerve involvement or alternative diagnoses.
How Doctors Use Pain Patterns for Diagnosis
Physical examination remains the gold standard for varicocele diagnosis, but your pain description guides the process.
During evaluation, urologists assess:
- Pain quality: Dull vs sharp, throbbing vs stabbing
- Timing: Morning vs evening, constant vs intermittent
- Aggravating factors: Standing, exercise, heat exposure
- Relieving factors: Rest, lying down, scrotal support
- Duration: Recent onset vs chronic (months to years)
Physical examination in standing and supine positions, with and without Valsalva maneuver, confirms varicocele grade. Doctors classify varicoceles as Grade 1 (palpable only during Valsalva), Grade 2 (easily palpable but not visible), or Grade 3 (easily visible).
Your pain pattern combined with physical findings determines whether imaging is necessary. Doppler ultrasound shows vein diameter and retrograde blood flow but isn’t required for all cases.
When Imaging Becomes Necessary
Doctors order scrotal ultrasound when:
- Physical exam findings don’t match pain description
- Pain is severe but varicocele grade seems mild
- Sharp or atypical pain suggests other conditions
- They need to rule out testicular tumors or other masses
Pain Patterns That Predict Treatment Success
Not all pain responds equally to treatment. Research identifies specific predictors:
High success predictors:
- Dull, aching pain worse with standing
- Pain duration longer than 3 months
- Pain localized to scrotum
- Grade 2-3 varicocele on exam
- Pain improves with scrotal support
Lower success predictors:
- Sharp pain radiating beyond scrotum
- Pain present less than 3 months
- Grade 1 (subclinical) varicocele
- Higher body mass index (BMI >22)
- Multiple pain locations
Why does longer pain duration predict better outcomes? It confirms the pain truly relates to the varicocele rather than temporary issues like minor trauma or muscle strain.
Conservative Management Based on Pain Type
Before considering surgery, doctors recommend conservative approaches for 3-6 months.
For dull ache patterns:
- Scrotal support through specialized underwear
- NSAIDs (ibuprofen, naproxen) for inflammation
- Limited heavy lifting and prolonged standing
- Ice therapy after exercise
Supportive underwear designed for varicocele provides gentle upward support that counteracts gravity’s effect on venous blood pooling. This varicocele support underwear combines lift with cooling technology to address both mechanical and temperature factors.
For sharp pain patterns:
Conservative treatment has lower success rates with sharp pain. Doctors move toward imaging and surgical consultation sooner because sharp pain may indicate complications requiring intervention.
Studies show conservative treatment resolves pain in 4-15% of men. Most require additional intervention.
When Different Pain Types Require Surgery
Surgical thresholds vary by pain pattern.
Dull pain: Try conservative treatment for 3-6 months first. If pain persists and affects quality of life, microsurgical varicocelectomy offers 80-90% pain resolution rates.
Sharp pain: Earlier surgical consultation is appropriate. Sharp pain suggests mechanical nerve compression or severe vein enlargement less likely to respond to conservative measures.
Intermittent vs constant: Constant pain indicates chronic venous pressure problems. Intermittent pain may respond better to lifestyle modifications and scrotal support before surgery.
Understanding Pain Mechanisms
What actually causes varicocele pain? Multiple factors contribute:
- Venous pressure: Blood pooling stretches vein walls, causing aching sensations
- Neural compression: Enlarged veins compress surrounding nerve fibers
- Temperature elevation: Poor venous drainage raises testicular temperature 2-3°C
- Oxidative stress: Impaired blood flow creates toxic metabolite buildup
- Testicular hypoxia: Reduced oxygen delivery damages tissue
These mechanisms explain why pain worsens with standing and improves with rest. Gravity increases venous pressure when upright. Lying down allows better venous drainage and reduced testicular temperature.
Other Symptoms That Accompany Different Pain Types
Pain rarely occurs alone. Associated symptoms provide diagnostic context:
With dull ache:
- Visible “bag of worms” veins
- Scrotal heaviness or fullness
- Gradual testicular size difference
- Reduced fertility parameters
With sharp pain:
- Sudden swelling episodes
- Testicular tenderness on touch
- Visible vein pulsation
- Nausea (rare, suggests emergency)
Document all symptoms for your doctor. The combination of pain type, associated symptoms, and physical findings creates your diagnostic picture.
Red Flags: When Pain Signals Emergency
Most varicocele pain develops gradually and isn’t emergent. However, certain patterns require immediate evaluation:
- Sudden onset severe pain
- Testicular swelling with nausea/vomiting
- Fever with scrotal pain
- Testicular mass you can feel
- Pain that prevents normal activities
These symptoms may indicate testicular torsion, infection, tumor, or other urgent conditions. Don’t assume everything is varicocele-related.
Frequently Asked Questions
Does varicocele pain mean it’s getting worse?
Not necessarily. Pain severity doesn’t always correlate with varicocele grade. You can have a Grade 3 varicocele with no pain or a Grade 1 with significant discomfort. Pain depends on individual nerve sensitivity and pain perception. However, new or worsening pain warrants medical evaluation to rule out complications.
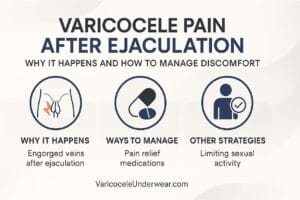
Can varicocele cause sharp pain during sex?
Yes, though it’s uncommon. Sexual activity increases blood flow and testicular movement, potentially causing sharp pain if you have varicocele. The increased venous pressure during arousal and ejaculation can trigger discomfort. If this occurs regularly, discuss it with your urologist as it may influence treatment decisions.
Why does my varicocele hurt more on hot days?
Heat causes blood vessels to dilate and impairs the cooling mechanisms your scrotum uses to regulate temperature. With varicocele, you already have impaired venous drainage. Heat compounds this problem by increasing blood volume in the already-enlarged veins, creating more pressure and pain.
Medical Review Note: This article is based on peer-reviewed medical literature and clinical guidelines. It provides educational information but doesn’t replace professional medical advice. Consult a urologist for evaluation of testicular pain or suspected varicocele.