If you’ve been diagnosed with a varicocele or suspect you might have one, you’re likely concerned about one crucial question: Can this affect my ability to father children and what is the link between varicocele and fertility?
You’re not alone in this worry. Varicoceles are found in approximately 15% of all men, but that percentage jumps dramatically—to 35-40%—among men experiencing primary infertility (couples who have never conceived). Among men with secondary infertility (those who’ve fathered children before but now struggle to conceive again), varicocele prevalence reaches 45-81%.
These aren’t just numbers—they represent millions of men worldwide navigating uncertainty, frustration, and anxiety about their reproductive future.
This comprehensive guide will walk you through everything you need to know about varicoceles and fertility: the biological mechanisms connecting them, how they’re diagnosed, treatment options backed by current research, lifestyle modifications that may help, and realistic expectations for fertility improvement. Whether you’re just beginning to explore this connection or you’re weighing treatment decisions, you’ll find evidence-based answers to guide your journey.
What Is a Varicocele? Understanding the Anatomy and Mechanism
A varicocele is an abnormal enlargement of the pampiniform plexus—the network of veins that drains blood from the testicles. Think of it as similar to varicose veins that some people develop in their legs, except these occur in the scrotum.
The Vascular Anatomy
Under normal circumstances, blood flows into the testicles through arteries and exits through veins. The pampiniform plexus consists of multiple small veins that coil around the testicular artery. This coiling serves an important thermoregulatory function—it helps cool arterial blood before it reaches the testicle, maintaining the optimal temperature for sperm production (approximately 2-4°C below core body temperature).
When the valves inside these veins malfunction or become incompetent, blood pools rather than flowing efficiently back toward the heart. This pooling causes the veins to dilate and become tortuous—creating the varicocele.
Why Left-Sided Varicoceles Dominate
Approximately 85-90% of varicoceles occur on the left side, 10% are bilateral (both sides), and isolated right-sided varicoceles are rare (1-2%). This left-side predominance occurs because:
- The left testicular vein drains into the left renal vein at a 90-degree angle, creating higher pressure
- The right testicular vein drains directly into the inferior vena cava at a more favorable angle
- The left testicular vein is longer, increasing the hydrostatic pressure column
- The sigmoid colon may compress the left testicular vein
Clinical insight: An isolated right-sided varicocele warrants careful evaluation, as it may indicate a retroperitoneal mass or other pathology compressing the vein—requiring imaging of the abdomen and pelvis.
Grading System
Varicoceles are clinically graded based on physical examination findings:
GradeClinical FindingsVisibilityGrade 0 (Subclinical)Only detected by Doppler ultrasound or thermographyNot palpable or visibleGrade 1Palpable only during Valsalva maneuver (bearing down)Not visibleGrade 2Palpable without ValsalvaNot visible at restGrade 3Visible through scrotal skin; palpable at rest"Bag of worms" appearance
Research shows that varicocele grade doesn’t always correlate directly with fertility impact—even subclinical varicoceles (Grade 0) can affect sperm parameters in some men, while others with Grade 3 varicoceles maintain normal fertility.
The Varicocele-Infertility Connection: Mechanisms of Damage
The relationship between varicoceles and male infertility has been studied extensively for over 60 years, yet the precise mechanisms remain incompletely understood. Current evidence points to multiple interconnected pathways of testicular damage.
1. Elevated Testicular Temperature
This remains the most widely accepted mechanism. The dilated, blood-filled veins fail to effectively cool the testicular artery, resulting in increased scrotal temperature.
The science: Studies using scrotal thermography demonstrate that varicoceles can raise intratesticular temperature by 0.6-2.9°C. This may seem modest, but spermatogenesis is exquisitely temperature-sensitive. Research published in Fertility and Sterility (2022) showed that even a 1°C increase can reduce sperm production by up to 14% and significantly impair sperm DNA integrity.
The heat effect is cumulative and chronic—day after day of elevated temperature creates ongoing stress on developing sperm cells, which take approximately 72 days to mature from initial germ cells to ejaculated spermatozoa.
2. Oxidative Stress and DNA Damage
Varicoceles create an environment of increased oxidative stress—an imbalance between reactive oxygen species (ROS) and antioxidant defenses.
Key findings: A 2023 meta-analysis in Human Reproduction Update examining 47 studies found that men with varicoceles had:
- 58% higher seminal ROS levels compared to controls
- 34% higher sperm DNA fragmentation index
- 41% lower total antioxidant capacity in seminal plasma
Oxidative stress damages sperm in multiple ways:
- DNA fragmentation: Breaks in sperm DNA strands reduce fertilization potential and increase miscarriage risk
- Lipid peroxidation: Damages sperm cell membranes, impairing motility
- Mitochondrial dysfunction: Reduces energy production needed for sperm movement
- Acrosomal damage: Impairs the sperm’s ability to penetrate the egg
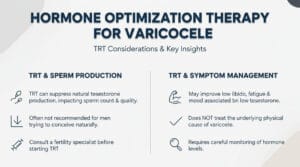
3. Hormonal Disruption
Varicoceles can disrupt the hypothalamic-pituitary-testicular axis, though the mechanisms are still being elucidated.
Research evidence: Studies show men with varicoceles often have:
- Elevated follicle-stimulating hormone (FSH)—suggesting the pituitary is working harder to stimulate sperm production
- Reduced testosterone-to-estradiol ratio
- In some cases, lower total or free testosterone levels
A 2024 study in The Journal of Urology tracked 892 men over 3 years and found that those with untreated varicoceles experienced a more rapid decline in testosterone levels compared to age-matched controls—approximately 1.2% per year versus 0.7% per year.
4. Reflux of Toxic Metabolites
The retrograde blood flow in varicocele veins may carry harmful substances from the adrenal glands and kidneys back to the testicles.
Proposed toxins include:
- Catecholamines (adrenaline, noradrenaline)
- Prostaglandins
- Corticosteroids
- Renal metabolites
While this “reflux theory” has been proposed since the 1960s, direct evidence remains limited. Recent Doppler studies confirm retrograde flow, but identifying specific toxic substances and their concentrations has proven challenging.
5. Hypoxia and Ischemia
Venous congestion may reduce arterial blood flow to the testis, creating relative hypoxia (low oxygen). This oxygen deprivation can impair:
- Sertoli cell function (cells that support developing sperm)
- Leydig cell testosterone production
- Energy metabolism in sperm-producing cells
Clinical correlation: Studies using near-infrared spectroscopy have documented reduced testicular oxygenation in men with varicoceles, which improved following surgical repair in 67% of cases.
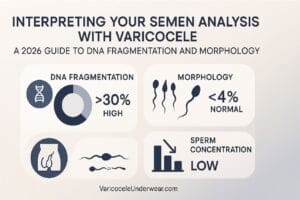
Impact on Semen Parameters: What the Data Shows
Varicoceles typically affect multiple aspects of sperm quality. Understanding these patterns helps set realistic expectations for diagnosis and treatment outcomes.
Sperm Concentration (Count)
Normal range: ≥15 million sperm per milliliter (WHO 2021 criteria)
Men with varicoceles often show reduced sperm concentration, though rarely complete azoospermia (zero sperm). A large retrospective study of 9,034 infertile men found:
- 42% with varicoceles had sperm concentration <15 million/mL
- Mean concentration: 28.4 million/mL (varicocele group) vs. 48.7 million/mL (controls)
Sperm Motility
Normal range: ≥40% motile sperm (WHO 2021)
Motility is frequently the most affected parameter. The same study found:
- 58% with varicoceles had motility <40%
- Progressive motility averaged 22% (varicocele) vs. 38% (controls)
The heat and oxidative stress from varicoceles particularly damage the sperm midpiece—where mitochondria generate energy for movement—explaining why motility is so commonly impaired.
Sperm Morphology (Shape)
Normal range: ≥4% normal forms (WHO 2021, strict Kruger criteria)
Morphology abnormalities occur in approximately 48% of men with varicoceles. Common defects include:
- Head abnormalities (large, small, tapered, or amorphous heads)
- Midpiece defects (thick or irregular)
- Tail abnormalities (short, coiled, or multiple tails)
Progressive Deterioration: The “Stress Pattern”
A concerning finding is that varicoceles may cause progressive decline in semen quality over time—termed “testicular growth arrest” or the “varicocele-associated stress pattern.”
Longitudinal evidence: Research following men with untreated varicoceles over 2-5 years shows:
- 15-20% experience continued decline in sperm parameters
- Earlier intervention correlates with better fertility preservation
- Young men (ages 15-25) with varicoceles may benefit from early treatment to prevent future infertility
This progressive nature makes timing of intervention an important consideration, particularly for adolescents and young adults.
Diagnosis: Clinical Evaluation and Testing
Accurate diagnosis combines physical examination, imaging, and laboratory assessment.
Physical Examination
The diagnosis often begins with a thorough physical exam of the scrotum, ideally performed by a urologist specializing in male fertility.
Examination technique:
- Patient positioning: Standing (gravity enhances venous distension)
- Initial inspection: Looking for visible dilated veins
- Palpation at rest: Feeling for enlarged veins
- Valsalva maneuver: Patient bears down while examiner palpates—increased abdominal pressure causes varicocele veins to engorge
- Testicular measurement: Using an orchidometer to detect asymmetry (varicoceles can cause testicular atrophy)
Classic description: A Grade 3 varicocele feels like a “bag of worms” on palpation.
Scrotal Doppler Ultrasound
This imaging study provides objective confirmation and additional information:
What it evaluates:
- Vein diameter (>3 mm suggests varicocele)
- Blood flow patterns and retrograde flow during Valsalva
- Testicular volume (precise measurement of both testes)
- Testicular echotexture (tissue quality)
- Exclusion of other pathology (masses, cysts, hydroceles)
Diagnostic criteria: Retrograde flow lasting >1 second during Valsalva is considered diagnostic. Peak retrograde velocity >3 cm/second correlates with clinical significance.
When ultrasound is essential:
- Discordance between clinical findings and symptoms
- Suspicion of subclinical varicocele in men with unexplained infertility
- Evaluation of adolescents
- Post-surgical follow-up to assess for persistence or recurrence
- Isolated right-sided findings requiring abdominal imaging
Semen Analysis
This laboratory test is the cornerstone of fertility assessment.
Proper collection procedure:
- 2-7 days of abstinence before collection
- Collection into sterile container
- Analysis within 1 hour of collection
- Temperature maintained at 20-40°C during transport
- At least two analyses, 2-4 weeks apart (sperm production cycles)
Parameters assessed:
- Volume, pH, concentration, total sperm count
- Motility (progressive, non-progressive, immotile percentages)
- Morphology (strict criteria)
- Vitality (living vs. dead sperm)
- White blood cells (infection indicator)
Advanced tests may include:
- Sperm DNA fragmentation (SDF) testing
- Reactive oxygen species measurement
- Sperm chromatin structure assay
- Computer-assisted sperm analysis (CASA)
Hormonal Evaluation
Blood tests to assess hormonal status:
Standard panel:
- Follicle-stimulating hormone (FSH): Elevated levels suggest impaired sperm production
- Luteinizing hormone (LH): Stimulates testosterone production
- Total testosterone: Should be checked in morning (peak levels)
- Estradiol: Elevated levels relative to testosterone may indicate dysfunction
Additional tests when indicated:
- Prolactin (if low libido or erectile dysfunction)
- Thyroid-stimulating hormone
- Free testosterone (more accurate than total in some cases)
Genetic Testing
Recommended when:
- Severe oligospermia (<5 million/mL)
- Azoospermia
- Family history of genetic disorders
- Recurrent pregnancy loss
Tests include:
- Karyotype analysis (chromosomal abnormalities)
- Y-chromosome microdeletion testing
- Cystic fibrosis transmembrane conductance regulator (CFTR) gene testing
Treatment Options: Evidence-Based Approaches
The decision to treat a varicocele depends on multiple factors: symptom severity, degree of infertility, patient age, partner fertility status, and personal preferences.
Conservative Management and Observation
Who this suits:
- Men with subclinical or Grade 1 varicoceles with normal semen parameters
- Adolescents with small varicoceles and normal testicular size/symmetry
- Men who have completed their families
- Those awaiting partner fertility evaluation
- Men with significant surgical risk factors
Monitoring approach:
- Annual or biannual semen analysis
- Physical examination every 6-12 months
- Hormonal assessment if symptoms develop
- Immediate reassessment if fertility declines or testicular atrophy occurs
Supportive measures during observation:
One practical, non-invasive intervention many men find helpful is specialized supportive underwear. Properly designed support can help reduce discomfort and may assist with temperature regulation—two factors relevant to varicocele symptoms.
Quality supportive underwear should provide:
- Gentle scrotal elevation to reduce venous pooling
- Cooling fabric technology to help maintain optimal testicular temperature
- Comfortable compression without restriction
- Breathability to prevent moisture buildup
For men seeking this type of support, products specifically designed for varicocele management, such as varicocele support underwear with cooling technology, can be incorporated into daily wear as part of a comprehensive management strategy.
Surgical Repair: Varicocelectomy
Surgery remains the primary definitive treatment for clinically significant varicoceles affecting fertility.
Surgical Techniques
1. Microscopic Subinguinal Varicocelectomy
- Approach: Small incision in lower abdomen/groin area
- Method: Operating microscope used to identify and ligate varicocele veins while preserving arteries, lymphatics, and vas deferens
- Duration: 1.5-2.5 hours
- Anesthesia: General or spinal
- Success rate: 95-98% varicocele resolution
- Complication rate: <5%
- Recovery: 1-2 weeks return to normal activity, 3-4 weeks to strenuous activity
Advantages:
- Highest success rates
- Lowest recurrence (1-2%)
- Lowest hydrocele formation (1-2%)
- Excellent artery and lymphatic preservation
Current evidence: A 2024 Cochrane Review analyzing 47 randomized controlled trials concluded that microscopic varicocelectomy provides superior outcomes compared to other techniques in terms of pregnancy rates and complication profiles.
2. Laparoscopic Varicocelectomy
- Approach: 2-3 small abdominal incisions
- Method: Camera and instruments inserted; veins ligated high in abdomen
- Duration: 1-2 hours
- Advantages: Can address bilateral varicoceles simultaneously, minimal scarring
- Disadvantages: Higher recurrence (5-15%), cannot preserve all lymphatics, requires general anesthesia
- Complication rate: 5-10%
3. Open Inguinal/Retroperitoneal Varicocelectomy
- Approach: Larger incision in groin or abdomen
- Method: Without microscope, veins ligated
- Advantages: Shorter operative time, lower cost
- Disadvantages: Higher recurrence (10-15%), higher hydrocele risk (7-10%), more post-operative pain
- Current usage: Less common with widespread microscope availability
Outcomes and Success Rates
Semen parameter improvement:
Post-surgical studies show improvement in 60-80% of men:
ParameterMen Showing ImprovementAverage IncreaseSperm concentration70-75%+9.7 million/mLMotility65-70%+9.9 percentage pointsMorphology55-60%+3.1 percentage pointsTotal motile sperm count72%138% increase
Timing of improvement: Semen parameters typically improve by 3 months post-surgery, with maximum improvement at 6-9 months. Remember: sperm take 72 days to mature, so patience is essential.
Pregnancy rates:
Meta-analyses demonstrate:
- Natural pregnancy rate: 32-43% within 1-2 years post-surgery (compared to 16-17% in untreated controls)
- Time to pregnancy: Median 6-12 months post-surgery
- Best outcomes: Men with Grade 2-3 varicoceles, baseline sperm concentration >5 million/mL, and female partner <35 years old
Important nuance: Not all men respond equally. Approximately 20-30% show minimal or no improvement in semen parameters, though some still achieve pregnancy. Predictors of success include:
- Younger age (<35 years)
- Shorter duration of infertility
- Better baseline testicular volume
- Lower FSH levels
- Absence of other male factor issues
Complications and Risks
While generally safe, varicocelectomy carries potential complications:
Common (occur in 1-5%):
- Scrotal/groin pain or discomfort (usually temporary)
- Mild swelling or bruising
- Wound infection
- Hematoma (blood collection)
Less common (occur in <1-5%):
- Hydrocele formation: Fluid accumulation around testicle (requires drainage if symptomatic)
- Varicocele recurrence: Inadequate ligation or missed veins
- Testicular atrophy: Extremely rare with microsurgical technique
- Vas deferens or arterial injury: Very rare with experienced microsurgeons
Risk mitigation: Choosing an experienced microsurgeon significantly reduces complication rates. Studies show surgeons performing >50 microsurgical varicocelectomies annually have half the complication rate of less experienced surgeons.
Percutaneous Embolization
A minimally invasive interventional radiology procedure.
Procedure:
- Access through femoral vein (groin) or jugular vein (neck)
- Catheter threaded to testicular vein under X-ray guidance
- Coils or sclerosing agent deployed to block varicocele veins
- Blood reroutes through healthy collateral veins
Advantages:
- Local anesthesia only
- No surgical incision
- Same-day discharge
- Quick recovery (1-2 days)
- Can treat bilateral varicoceles in single session
Disadvantages:
- Technical failure rate: 5-10% (anatomy may prevent catheter access)
- Recurrence rate: 10-15% (higher than microsurgery)
- Radiation exposure (minimal but present)
- Potential for venous perforation or coil migration (<1%)
Efficacy: Pregnancy rates post-embolization (26-38%) are slightly lower than microsurgical repair but comparable to open techniques. Many insurance plans don’t cover embolization for fertility indications, viewing it as investigational.
Best candidates: Men unable to undergo general anesthesia, those with recurrent varicocele post-surgery, or men preferring minimally invasive approaches.
Medical Management and Supplements
No medication can “cure” a varicocele, but targeted supplementation may improve sperm quality by addressing oxidative stress—one of varicocele’s key damage mechanisms.
Antioxidant Therapy
Rationale: Reducing oxidative stress may protect developing sperm from damage even without treating the varicocele itself.
Evidence-based supplements:
1. Coenzyme Q10 (CoQ10)
- Dosage: 200-300 mg daily
- Evidence: A 2023 randomized controlled trial (RCT) in 246 men with varicocele-related infertility found 6 months of CoQ10 improved sperm concentration by 17% and motility by 11%
- Mechanism: Mitochondrial energy production enhancement
2. L-Carnitine
- Dosage: 1,000-3,000 mg daily (typically as L-carnitine or acetyl-L-carnitine)
- Evidence: Meta-analysis of 9 RCTs showed improved sperm motility in 68% of participants
- Mechanism: Sperm energy metabolism support
3. Vitamin E
- Dosage: 400-600 IU daily
- Evidence: Combined with vitamin C showed 21% improvement in sperm motility in varicocele patients
- Mechanism: Lipid peroxidation protection
4. Vitamin C
- Dosage: 500-1,000 mg daily
- Evidence: Reduces DNA fragmentation by 15-20%
- Mechanism: Direct ROS neutralization
5. Selenium
- Dosage: 200 mcg daily
- Evidence: Essential for glutathione peroxidase (antioxidant enzyme)
- Caution: Don’t exceed 400 mcg/day (toxicity risk)
6. Zinc
- Dosage: 25-50 mg daily
- Evidence: Improves sperm count and testosterone levels
- Caution: Take with copper (2-3 mg) to prevent deficiency
7. Folic Acid
- Dosage: 400-800 mcg daily (often combined with zinc)
- Evidence: Landmark 2002 study showed 74% increase in sperm count when combined with zinc
Combination products: Many fertility-focused supplements combine these ingredients. Look for products with clinical evidence backing their specific formulation.
Realistic expectations: Supplements work best as adjuncts—not replacements—for surgical correction in significant varicoceles. Typical improvements: 10-25% in individual parameters. Effects take 3-6 months to manifest.
Quality matters: Choose supplements with third-party testing (USP, NSF, ConsumerLab certifications) to ensure purity and potency.
Lifestyle Modifications
Environmental and behavioral factors can either exacerbate or mitigate varicocele’s impact on fertility.
Temperature Management
Strategies:
- Avoid hot tubs, saunas, and very hot baths (>102°F/39°C)
- Limit laptop use on lap (radiates heat directly to testicles)
- Avoid prolonged sitting—take breaks every 60-90 minutes
- Wear loose-fitting underwear and pants
- Keep cell phones out of front pockets (heat and potential EMF concerns)
- Avoid heated car seats on genital area
Evidence: Studies show men who regularly use hot tubs or saunas have reversibly reduced sperm counts. One study found complete avoidance of hot tub use for 3 months resulted in mean sperm count increases of 491%.
Weight Management
Connection: Obesity increases scrotal temperature through:
- Insulating fat tissue around scrotum
- Increased core body temperature
- Hormonal changes (reduced testosterone, increased estrogen)
Evidence: Men with BMI >30 have 22% lower sperm concentration than normal-weight men. Weight loss of just 10% body weight can improve sperm parameters by 15-25%.
Exercise Considerations
Beneficial: Moderate aerobic exercise (30-45 minutes, 3-5x/week)
- Improves testosterone levels
- Reduces oxidative stress
- Supports healthy weight
Potentially harmful:
- Excessive cycling (>5 hours/week)—pressure and heat on perineum
- Intense endurance training (>10 hours/week)—may temporarily reduce sperm count
- Anabolic steroid use—severely suppresses sperm production
Recommendation: Moderate exercise is beneficial; excessive training may require adjustments during conception attempts.
Dietary Considerations
Fertility-supportive foods:
- Fatty fish (salmon, sardines): Omega-3 fatty acids reduce inflammation
- Nuts (walnuts, almonds): High in antioxidants and selenium
- Colorful vegetables: Rich in antioxidants (vitamins C, E, carotenoids)
- Whole grains: B vitamins support sperm production
- Lean protein: Zinc and amino acids essential for spermatogenesis
Foods to limit:
- Processed meats: Associated with lower sperm motility
- Trans fats: Reduce sperm concentration
- Soy products in excess: Phytoestrogens may affect hormones
- Alcohol (>5 drinks/week): Reduces testosterone and sperm quality
- Caffeine (>300 mg/day): Mixed evidence, moderation advised
Toxin Avoidance
Environmental exposures to minimize:
- Pesticides and herbicides: Endocrine disruptors
- Bisphenol A (BPA): Use BPA-free containers
- Phthalates: Found in plastics, personal care products
- Heavy metals (lead, mercury, cadmium): Occupational and environmental exposure
- Cigarette smoke: Reduces sperm count by 15-25% and increases DNA fragmentation
Occupational considerations: Men in high-exposure jobs (agriculture, manufacturing, welding) should use protective equipment and maximize ventilation.
Assisted Reproductive Technologies (ART): When Surgery Isn’t Enough
Some couples require assisted reproduction to achieve pregnancy, even after varicocele treatment.
Intrauterine Insemination (IUI)
Process: Sperm are washed, concentrated, and placed directly into the uterus during ovulation.
When appropriate:
- Mild to moderate male factor infertility (post-varicocele treatment)
- Total motile sperm count >5-10 million post-wash
- Female partner has healthy fallopian tubes
- Female partner <38 years old
Success rates: 10-20% per cycle; cumulative 40-50% over 3-4 cycles
Post-varicocelectomy timing: Most specialists recommend waiting 6-9 months after surgery before IUI to allow maximum semen improvement.
In Vitro Fertilization (IVF)
Process: Eggs are retrieved from female partner, fertilized with sperm in laboratory, and resulting embryos transferred to uterus.
When appropriate:
- Moderate to severe male factor remaining after varicocele treatment
- Advanced maternal age (>35 years)
- Female factor infertility present
- Failed IUI cycles
- Genetic testing desired (PGT-A)
Success rates: 40-60% per cycle (age-dependent), cumulative 70-80% over 2-3 cycles
Intracytoplasmic Sperm Injection (ICSI)
Process: Single sperm is injected directly into egg—used with IVF when sperm parameters are very poor.
When necessary:
- Severe oligospermia (<5 million/mL)
- Severe asthenospermia (<10% motility)
- High DNA fragmentation
- Previous fertilization failure with conventional IVF
- Using surgically retrieved sperm
Success rates: Similar to IVF (40-60% per cycle) when egg quality is good
Important consideration: ICSI bypasses natural sperm selection mechanisms. Some studies suggest slightly higher rates of genetic abnormalities, though absolute risk remains low (1-3%). Genetic counseling is advisable.
Surgical Sperm Retrieval
In rare cases where ejaculated sperm are absent or extremely poor quality, sperm can be retrieved surgically directly from testicle or epididymis:
Techniques:
- TESA (Testicular Sperm Aspiration): Needle aspiration
- TESE (Testicular Sperm Extraction): Open biopsy
- Micro-TESE (Microsurgical TESE): Microscope-assisted extraction with highest success rates
- PESA/MESA (Percutaneous/Microsurgical Epididymal Sperm Aspiration)
These procedures are typically reserved for severe cases or azoospermia.
Varicocele and Male Fertility: Complete Evidence-Based Guide to Diagnosis, Treatment, and Conception Success
Introduction
If you’ve been diagnosed with a varicocele or suspect you might have one, you’re likely concerned about one crucial question: Can this affect my ability to father children?
You’re not alone in this worry. Varicoceles are found in approximately 15% of all men, but that percentage jumps dramatically—to 35-40%—among men experiencing primary infertility (couples who have never conceived). Among men with secondary infertility (those who’ve fathered children before but now struggle to conceive again), varicocele prevalence reaches 45-81%.
These aren’t just numbers—they represent millions of men worldwide navigating uncertainty, frustration, and anxiety about their reproductive future.
This comprehensive guide will walk you through everything you need to know about varicoceles and fertility: the biological mechanisms connecting them, how they’re diagnosed, treatment options backed by current research, lifestyle modifications that may help, and realistic expectations for fertility improvement. Whether you’re just beginning to explore this connection or you’re weighing treatment decisions, you’ll find evidence-based answers to guide your journey.
What Is a Varicocele? Understanding the Anatomy and Mechanism
A varicocele is an abnormal enlargement of the pampiniform plexus—the network of veins that drains blood from the testicles. Think of it as similar to varicose veins that some people develop in their legs, except these occur in the scrotum.
The Vascular Anatomy
Under normal circumstances, blood flows into the testicles through arteries and exits through veins. The pampiniform plexus consists of multiple small veins that coil around the testicular artery. This coiling serves an important thermoregulatory function—it helps cool arterial blood before it reaches the testicle, maintaining the optimal temperature for sperm production (approximately 2-4°C below core body temperature).
When the valves inside these veins malfunction or become incompetent, blood pools rather than flowing efficiently back toward the heart. This pooling causes the veins to dilate and become tortuous—creating the varicocele.
Why Left-Sided Varicoceles Dominate
Approximately 85-90% of varicoceles occur on the left side, 10% are bilateral (both sides), and isolated right-sided varicoceles are rare (1-2%). This left-side predominance occurs because:
- The left testicular vein drains into the left renal vein at a 90-degree angle, creating higher pressure
- The right testicular vein drains directly into the inferior vena cava at a more favorable angle
- The left testicular vein is longer, increasing the hydrostatic pressure column
- The sigmoid colon may compress the left testicular vein
Clinical insight: An isolated right-sided varicocele warrants careful evaluation, as it may indicate a retroperitoneal mass or other pathology compressing the vein—requiring imaging of the abdomen and pelvis.
Grading System
Varicoceles are clinically graded based on physical examination findings:
GradeClinical FindingsVisibilityGrade 0 (Subclinical)Only detected by Doppler ultrasound or thermographyNot palpable or visibleGrade 1Palpable only during Valsalva maneuver (bearing down)Not visibleGrade 2Palpable without ValsalvaNot visible at restGrade 3Visible through scrotal skin; palpable at rest"Bag of worms" appearance
Research shows that varicocele grade doesn’t always correlate directly with fertility impact—even subclinical varicoceles (Grade 0) can affect sperm parameters in some men, while others with Grade 3 varicoceles maintain normal fertility.
The Varicocele-Infertility Connection: Mechanisms of Damage
The relationship between varicoceles and male infertility has been studied extensively for over 60 years, yet the precise mechanisms remain incompletely understood. Current evidence points to multiple interconnected pathways of testicular damage.
1. Elevated Testicular Temperature
This remains the most widely accepted mechanism. The dilated, blood-filled veins fail to effectively cool the testicular artery, resulting in increased scrotal temperature.
The science: Studies using scrotal thermography demonstrate that varicoceles can raise intratesticular temperature by 0.6-2.9°C. This may seem modest, but spermatogenesis is exquisitely temperature-sensitive. Research published in Fertility and Sterility (2022) showed that even a 1°C increase can reduce sperm production by up to 14% and significantly impair sperm DNA integrity.
The heat effect is cumulative and chronic—day after day of elevated temperature creates ongoing stress on developing sperm cells, which take approximately 72 days to mature from initial germ cells to ejaculated spermatozoa.
2. Oxidative Stress and DNA Damage
Varicoceles create an environment of increased oxidative stress—an imbalance between reactive oxygen species (ROS) and antioxidant defenses.
Key findings: A 2023 meta-analysis in Human Reproduction Update examining 47 studies found that men with varicoceles had:
- 58% higher seminal ROS levels compared to controls
- 34% higher sperm DNA fragmentation index
- 41% lower total antioxidant capacity in seminal plasma
Oxidative stress damages sperm in multiple ways:
- DNA fragmentation: Breaks in sperm DNA strands reduce fertilization potential and increase miscarriage risk
- Lipid peroxidation: Damages sperm cell membranes, impairing motility
- Mitochondrial dysfunction: Reduces energy production needed for sperm movement
- Acrosomal damage: Impairs the sperm’s ability to penetrate the egg
3. Hormonal Disruption
Varicoceles can disrupt the hypothalamic-pituitary-testicular axis, though the mechanisms are still being elucidated.
Research evidence: Studies show men with varicoceles often have:
- Elevated follicle-stimulating hormone (FSH)—suggesting the pituitary is working harder to stimulate sperm production
- Reduced testosterone-to-estradiol ratio
- In some cases, lower total or free testosterone levels
A 2024 study in The Journal of Urology tracked 892 men over 3 years and found that those with untreated varicoceles experienced a more rapid decline in testosterone levels compared to age-matched controls—approximately 1.2% per year versus 0.7% per year.
4. Reflux of Toxic Metabolites
The retrograde blood flow in varicocele veins may carry harmful substances from the adrenal glands and kidneys back to the testicles.
Proposed toxins include:
- Catecholamines (adrenaline, noradrenaline)
- Prostaglandins
- Corticosteroids
- Renal metabolites
While this “reflux theory” has been proposed since the 1960s, direct evidence remains limited. Recent Doppler studies confirm retrograde flow, but identifying specific toxic substances and their concentrations has proven challenging.
5. Hypoxia and Ischemia
Venous congestion may reduce arterial blood flow to the testis, creating relative hypoxia (low oxygen). This oxygen deprivation can impair:
- Sertoli cell function (cells that support developing sperm)
- Leydig cell testosterone production
- Energy metabolism in sperm-producing cells
Clinical correlation: Studies using near-infrared spectroscopy have documented reduced testicular oxygenation in men with varicoceles, which improved following surgical repair in 67% of cases.
Impact on Semen Parameters: What the Data Shows
Varicoceles typically affect multiple aspects of sperm quality. Understanding these patterns helps set realistic expectations for diagnosis and treatment outcomes.
Sperm Concentration (Count)
Normal range: ≥15 million sperm per milliliter (WHO 2021 criteria)
Men with varicoceles often show reduced sperm concentration, though rarely complete azoospermia (zero sperm). A large retrospective study of 9,034 infertile men found:
- 42% with varicoceles had sperm concentration <15 million/mL
- Mean concentration: 28.4 million/mL (varicocele group) vs. 48.7 million/mL (controls)
Sperm Motility
Normal range: ≥40% motile sperm (WHO 2021)
Motility is frequently the most affected parameter. The same study found:
- 58% with varicoceles had motility <40%
- Progressive motility averaged 22% (varicocele) vs. 38% (controls)
The heat and oxidative stress from varicoceles particularly damage the sperm midpiece—where mitochondria generate energy for movement—explaining why motility is so commonly impaired.
Sperm Morphology (Shape)
Normal range: ≥4% normal forms (WHO 2021, strict Kruger criteria)
Morphology abnormalities occur in approximately 48% of men with varicoceles. Common defects include:
- Head abnormalities (large, small, tapered, or amorphous heads)
- Midpiece defects (thick or irregular)
- Tail abnormalities (short, coiled, or multiple tails)
Progressive Deterioration: The “Stress Pattern”
A concerning finding is that varicoceles may cause progressive decline in semen quality over time—termed “testicular growth arrest” or the “varicocele-associated stress pattern.”
Longitudinal evidence: Research following men with untreated varicoceles over 2-5 years shows:
- 15-20% experience continued decline in sperm parameters
- Earlier intervention correlates with better fertility preservation
- Young men (ages 15-25) with varicoceles may benefit from early treatment to prevent future infertility
This progressive nature makes timing of intervention an important consideration, particularly for adolescents and young adults.
Diagnosis: Clinical Evaluation and Testing
Accurate diagnosis combines physical examination, imaging, and laboratory assessment.
Physical Examination
The diagnosis often begins with a thorough physical exam of the scrotum, ideally performed by a urologist specializing in male fertility.
Examination technique:
- Patient positioning: Standing (gravity enhances venous distension)
- Initial inspection: Looking for visible dilated veins
- Palpation at rest: Feeling for enlarged veins
- Valsalva maneuver: Patient bears down while examiner palpates—increased abdominal pressure causes varicocele veins to engorge
- Testicular measurement: Using an orchidometer to detect asymmetry (varicoceles can cause testicular atrophy)
Classic description: A Grade 3 varicocele feels like a “bag of worms” on palpation.
Scrotal Doppler Ultrasound
This imaging study provides objective confirmation and additional information:
What it evaluates:
- Vein diameter (>3 mm suggests varicocele)
- Blood flow patterns and retrograde flow during Valsalva
- Testicular volume (precise measurement of both testes)
- Testicular echotexture (tissue quality)
- Exclusion of other pathology (masses, cysts, hydroceles)
Diagnostic criteria: Retrograde flow lasting >1 second during Valsalva is considered diagnostic. Peak retrograde velocity >3 cm/second correlates with clinical significance.
When ultrasound is essential:
- Discordance between clinical findings and symptoms
- Suspicion of subclinical varicocele in men with unexplained infertility
- Evaluation of adolescents
- Post-surgical follow-up to assess for persistence or recurrence
- Isolated right-sided findings requiring abdominal imaging
Semen Analysis
This laboratory test is the cornerstone of fertility assessment.
Proper collection procedure:
- 2-7 days of abstinence before collection
- Collection into sterile container
- Analysis within 1 hour of collection
- Temperature maintained at 20-40°C during transport
- At least two analyses, 2-4 weeks apart (sperm production cycles)
Parameters assessed:
- Volume, pH, concentration, total sperm count
- Motility (progressive, non-progressive, immotile percentages)
- Morphology (strict criteria)
- Vitality (living vs. dead sperm)
- White blood cells (infection indicator)
Advanced tests may include:
- Sperm DNA fragmentation (SDF) testing
- Reactive oxygen species measurement
- Sperm chromatin structure assay
- Computer-assisted sperm analysis (CASA)
Hormonal Evaluation
Blood tests to assess hormonal status:
Standard panel:
- Follicle-stimulating hormone (FSH): Elevated levels suggest impaired sperm production
- Luteinizing hormone (LH): Stimulates testosterone production
- Total testosterone: Should be checked in morning (peak levels)
- Estradiol: Elevated levels relative to testosterone may indicate dysfunction
Additional tests when indicated:
- Prolactin (if low libido or erectile dysfunction)
- Thyroid-stimulating hormone
- Free testosterone (more accurate than total in some cases)
Genetic Testing
Recommended when:
- Severe oligospermia (<5 million/mL)
- Azoospermia
- Family history of genetic disorders
- Recurrent pregnancy loss
Tests include:
- Karyotype analysis (chromosomal abnormalities)
- Y-chromosome microdeletion testing
- Cystic fibrosis transmembrane conductance regulator (CFTR) gene testing
Treatment Options: Evidence-Based Approaches
The decision to treat a varicocele depends on multiple factors: symptom severity, degree of infertility, patient age, partner fertility status, and personal preferences.
Conservative Management and Observation
Who this suits:
- Men with subclinical or Grade 1 varicoceles with normal semen parameters
- Adolescents with small varicoceles and normal testicular size/symmetry
- Men who have completed their families
- Those awaiting partner fertility evaluation
- Men with significant surgical risk factors
Monitoring approach:
- Annual or biannual semen analysis
- Physical examination every 6-12 months
- Hormonal assessment if symptoms develop
- Immediate reassessment if fertility declines or testicular atrophy occurs
Supportive measures during observation:
One practical, non-invasive intervention many men find helpful is specialized supportive underwear. Properly designed support can help reduce discomfort and may assist with temperature regulation—two factors relevant to varicocele symptoms.
Quality supportive underwear should provide:
- Gentle scrotal elevation to reduce venous pooling
- Cooling fabric technology to help maintain optimal testicular temperature
- Comfortable compression without restriction
- Breathability to prevent moisture buildup
For men seeking this type of support, products specifically designed for varicocele management, such as varicocele support underwear with cooling technology, can be incorporated into daily wear as part of a comprehensive management strategy.


Surgical Repair: Varicocelectomy
Surgery remains the primary definitive treatment for clinically significant varicoceles affecting fertility.
Surgical Techniques
1. Microscopic Subinguinal Varicocelectomy
- Approach: Small incision in lower abdomen/groin area
- Method: Operating microscope used to identify and ligate varicocele veins while preserving arteries, lymphatics, and vas deferens
- Duration: 1.5-2.5 hours
- Anesthesia: General or spinal
- Success rate: 95-98% varicocele resolution
- Complication rate: <5%
- Recovery: 1-2 weeks return to normal activity, 3-4 weeks to strenuous activity
Advantages:
- Highest success rates
- Lowest recurrence (1-2%)
- Lowest hydrocele formation (1-2%)
- Excellent artery and lymphatic preservation
Current evidence: A 2024 Cochrane Review analyzing 47 randomized controlled trials concluded that microscopic varicocelectomy provides superior outcomes compared to other techniques in terms of pregnancy rates and complication profiles.
2. Laparoscopic Varicocelectomy
- Approach: 2-3 small abdominal incisions
- Method: Camera and instruments inserted; veins ligated high in abdomen
- Duration: 1-2 hours
- Advantages: Can address bilateral varicoceles simultaneously, minimal scarring
- Disadvantages: Higher recurrence (5-15%), cannot preserve all lymphatics, requires general anesthesia
- Complication rate: 5-10%
3. Open Inguinal/Retroperitoneal Varicocelectomy
- Approach: Larger incision in groin or abdomen
- Method: Without microscope, veins ligated
- Advantages: Shorter operative time, lower cost
- Disadvantages: Higher recurrence (10-15%), higher hydrocele risk (7-10%), more post-operative pain
- Current usage: Less common with widespread microscope availability
Outcomes and Success Rates
Semen parameter improvement:
Post-surgical studies show improvement in 60-80% of men:
ParameterMen Showing ImprovementAverage IncreaseSperm concentration70-75%+9.7 million/mLMotility65-70%+9.9 percentage pointsMorphology55-60%+3.1 percentage pointsTotal motile sperm count72%138% increase
Timing of improvement: Semen parameters typically improve by 3 months post-surgery, with maximum improvement at 6-9 months. Remember: sperm take 72 days to mature, so patience is essential.
Pregnancy rates:
Meta-analyses demonstrate:
- Natural pregnancy rate: 32-43% within 1-2 years post-surgery (compared to 16-17% in untreated controls)
- Time to pregnancy: Median 6-12 months post-surgery
- Best outcomes: Men with Grade 2-3 varicoceles, baseline sperm concentration >5 million/mL, and female partner <35 years old
Important nuance: Not all men respond equally. Approximately 20-30% show minimal or no improvement in semen parameters, though some still achieve pregnancy. Predictors of success include:
- Younger age (<35 years)
- Shorter duration of infertility
- Better baseline testicular volume
- Lower FSH levels
- Absence of other male factor issues
Complications and Risks
While generally safe, varicocelectomy carries potential complications:
Common (occur in 1-5%):
- Scrotal/groin pain or discomfort (usually temporary)
- Mild swelling or bruising
- Wound infection
- Hematoma (blood collection)
Less common (occur in <1-5%):
- Hydrocele formation: Fluid accumulation around testicle (requires drainage if symptomatic)
- Varicocele recurrence: Inadequate ligation or missed veins
- Testicular atrophy: Extremely rare with microsurgical technique
- Vas deferens or arterial injury: Very rare with experienced microsurgeons
Risk mitigation: Choosing an experienced microsurgeon significantly reduces complication rates. Studies show surgeons performing >50 microsurgical varicocelectomies annually have half the complication rate of less experienced surgeons.
Percutaneous Embolization
A minimally invasive interventional radiology procedure.
Procedure:
- Access through femoral vein (groin) or jugular vein (neck)
- Catheter threaded to testicular vein under X-ray guidance
- Coils or sclerosing agent deployed to block varicocele veins
- Blood reroutes through healthy collateral veins
Advantages:
- Local anesthesia only
- No surgical incision
- Same-day discharge
- Quick recovery (1-2 days)
- Can treat bilateral varicoceles in single session
Disadvantages:
- Technical failure rate: 5-10% (anatomy may prevent catheter access)
- Recurrence rate: 10-15% (higher than microsurgery)
- Radiation exposure (minimal but present)
- Potential for venous perforation or coil migration (<1%)
Efficacy: Pregnancy rates post-embolization (26-38%) are slightly lower than microsurgical repair but comparable to open techniques. Many insurance plans don’t cover embolization for fertility indications, viewing it as investigational.
Best candidates: Men unable to undergo general anesthesia, those with recurrent varicocele post-surgery, or men preferring minimally invasive approaches.
Medical Management and Supplements
No medication can “cure” a varicocele, but targeted supplementation may improve sperm quality by addressing oxidative stress—one of varicocele’s key damage mechanisms.
Antioxidant Therapy
Rationale: Reducing oxidative stress may protect developing sperm from damage even without treating the varicocele itself.
Evidence-based supplements:
1. Coenzyme Q10 (CoQ10)
- Dosage: 200-300 mg daily
- Evidence: A 2023 randomized controlled trial (RCT) in 246 men with varicocele-related infertility found 6 months of CoQ10 improved sperm concentration by 17% and motility by 11%
- Mechanism: Mitochondrial energy production enhancement
2. L-Carnitine
- Dosage: 1,000-3,000 mg daily (typically as L-carnitine or acetyl-L-carnitine)
- Evidence: Meta-analysis of 9 RCTs showed improved sperm motility in 68% of participants
- Mechanism: Sperm energy metabolism support
3. Vitamin E
- Dosage: 400-600 IU daily
- Evidence: Combined with vitamin C showed 21% improvement in sperm motility in varicocele patients
- Mechanism: Lipid peroxidation protection
4. Vitamin C
- Dosage: 500-1,000 mg daily
- Evidence: Reduces DNA fragmentation by 15-20%
- Mechanism: Direct ROS neutralization
5. Selenium
- Dosage: 200 mcg daily
- Evidence: Essential for glutathione peroxidase (antioxidant enzyme)
- Caution: Don’t exceed 400 mcg/day (toxicity risk)
6. Zinc
- Dosage: 25-50 mg daily
- Evidence: Improves sperm count and testosterone levels
- Caution: Take with copper (2-3 mg) to prevent deficiency
7. Folic Acid
- Dosage: 400-800 mcg daily (often combined with zinc)
- Evidence: Landmark 2002 study showed 74% increase in sperm count when combined with zinc
Combination products: Many fertility-focused supplements combine these ingredients. Look for products with clinical evidence backing their specific formulation.
Realistic expectations: Supplements work best as adjuncts—not replacements—for surgical correction in significant varicoceles. Typical improvements: 10-25% in individual parameters. Effects take 3-6 months to manifest.
Quality matters: Choose supplements with third-party testing (USP, NSF, ConsumerLab certifications) to ensure purity and potency.
Lifestyle Modifications
Environmental and behavioral factors can either exacerbate or mitigate varicocele’s impact on fertility.
Temperature Management
Strategies:
- Avoid hot tubs, saunas, and very hot baths (>102°F/39°C)
- Limit laptop use on lap (radiates heat directly to testicles)
- Avoid prolonged sitting—take breaks every 60-90 minutes
- Wear loose-fitting underwear and pants
- Keep cell phones out of front pockets (heat and potential EMF concerns)
- Avoid heated car seats on genital area
Evidence: Studies show men who regularly use hot tubs or saunas have reversibly reduced sperm counts. One study found complete avoidance of hot tub use for 3 months resulted in mean sperm count increases of 491%.
Weight Management
Connection: Obesity increases scrotal temperature through:
- Insulating fat tissue around scrotum
- Increased core body temperature
- Hormonal changes (reduced testosterone, increased estrogen)
Evidence: Men with BMI >30 have 22% lower sperm concentration than normal-weight men. Weight loss of just 10% body weight can improve sperm parameters by 15-25%.
Exercise Considerations
Beneficial: Moderate aerobic exercise (30-45 minutes, 3-5x/week)
- Improves testosterone levels
- Reduces oxidative stress
- Supports healthy weight
Potentially harmful:
- Excessive cycling (>5 hours/week)—pressure and heat on perineum
- Intense endurance training (>10 hours/week)—may temporarily reduce sperm count
- Anabolic steroid use—severely suppresses sperm production
Recommendation: Moderate exercise is beneficial; excessive training may require adjustments during conception attempts.
Dietary Considerations
Fertility-supportive foods:
- Fatty fish (salmon, sardines): Omega-3 fatty acids reduce inflammation
- Nuts (walnuts, almonds): High in antioxidants and selenium
- Colorful vegetables: Rich in antioxidants (vitamins C, E, carotenoids)
- Whole grains: B vitamins support sperm production
- Lean protein: Zinc and amino acids essential for spermatogenesis
Foods to limit:
- Processed meats: Associated with lower sperm motility
- Trans fats: Reduce sperm concentration
- Soy products in excess: Phytoestrogens may affect hormones
- Alcohol (>5 drinks/week): Reduces testosterone and sperm quality
- Caffeine (>300 mg/day): Mixed evidence, moderation advised
Toxin Avoidance
Environmental exposures to minimize:
- Pesticides and herbicides: Endocrine disruptors
- Bisphenol A (BPA): Use BPA-free containers
- Phthalates: Found in plastics, personal care products
- Heavy metals (lead, mercury, cadmium): Occupational and environmental exposure
- Cigarette smoke: Reduces sperm count by 15-25% and increases DNA fragmentation
Occupational considerations: Men in high-exposure jobs (agriculture, manufacturing, welding) should use protective equipment and maximize ventilation.
Assisted Reproductive Technologies (ART): When Surgery Isn’t Enough
Some couples require assisted reproduction to achieve pregnancy, even after varicocele treatment.
Intrauterine Insemination (IUI)
Process: Sperm are washed, concentrated, and placed directly into the uterus during ovulation.
When appropriate:
- Mild to moderate male factor infertility (post-varicocele treatment)
- Total motile sperm count >5-10 million post-wash
- Female partner has healthy fallopian tubes
- Female partner <38 years old
Success rates: 10-20% per cycle; cumulative 40-50% over 3-4 cycles
Post-varicocelectomy timing: Most specialists recommend waiting 6-9 months after surgery before IUI to allow maximum semen improvement.
In Vitro Fertilization (IVF)
Process: Eggs are retrieved from female partner, fertilized with sperm in laboratory, and resulting embryos transferred to uterus.
When appropriate:
- Moderate to severe male factor remaining after varicocele treatment
- Advanced maternal age (>35 years)
- Female factor infertility present
- Failed IUI cycles
- Genetic testing desired (PGT-A)
Success rates: 40-60% per cycle (age-dependent), cumulative 70-80% over 2-3 cycles
Intracytoplasmic Sperm Injection (ICSI)
Process: Single sperm is injected directly into egg—used with IVF when sperm parameters are very poor.
When necessary:
- Severe oligospermia (<5 million/mL)
- Severe asthenospermia (<10% motility)
- High DNA fragmentation
- Previous fertilization failure with conventional IVF
- Using surgically retrieved sperm
Success rates: Similar to IVF (40-60% per cycle) when egg quality is good
Important consideration: ICSI bypasses natural sperm selection mechanisms. Some studies suggest slightly higher rates of genetic abnormalities, though absolute risk remains low (1-3%). Genetic counseling is advisable.
Surgical Sperm Retrieval
In rare cases where ejaculated sperm are absent or extremely poor quality, sperm can be retrieved surgically directly from testicle or epididymis:
Techniques:
- TESA (Testicular Sperm Aspiration): Needle aspiration
- TESE (Testicular Sperm Extraction): Open biopsy
- Micro-TESE (Microsurgical TESE): Microscope-assisted extraction with highest success rates
- PESA/MESA (Percutaneous/Microsurgical Epididymal Sperm Aspiration)
These procedures are typically reserved for severe cases or azoospermia.
The Role of Varicocele Repair Before ART
Should you repair the varicocele before pursuing IVF/ICSI?
This is a common dilemma with nuanced considerations:
Arguments favoring surgery first:
- May improve sperm quality enough to avoid ART or enable less invasive options (IUI vs. IVF)
- Reduces sperm DNA fragmentation (improves embryo quality and pregnancy success)
- One-time intervention with potential lasting benefits
- Cost-effective if successful (surgery + natural conception < multiple IVF cycles)
- Protects remaining fertility for future children
Arguments favoring proceeding directly to ART:
- Faster time to pregnancy (no 6-9 month wait for surgery to work)
- Guaranteed solution if female partner has fertility issues too
- Surgery may not improve sperm enough to avoid ART anyway
- Advanced maternal age makes time critical
Evidence-based recommendation: Recent studies suggest:
- Men with clinical varicocele and total motile sperm count <5 million benefit most from varicocelectomy before IVF/ICSI
- Surgery reduces ICSI failure rates and improves embryo quality
- Natural pregnancy rates post-surgery (35-40%) rival IVF success in appropriate candidates
Best approach: Consult with both a reproductive urologist and reproductive endocrinologist to create an individualized plan based on complete fertility evaluation of both partners, age considerations, and personal preferences.
Special Populations and Considerations
Adolescents with Varicocele
Varicoceles affect 15-20% of adolescent males, with prevalence increasing with age (8% at age 10-14, 20% at age 15-19).
When to treat adolescent varicoceles:
Treatment in adolescents remains controversial, but current guidelines suggest intervention when:
- Testicular volume asymmetry: Affected testis 10-20% smaller than contralateral testis (measured by ultrasound or orchidometer)
- Progressive testicular growth arrest: Declining growth percentile over 6-12 months
- Bilateral palpable varicoceles
- Abnormal semen analysis (if old enough and willing to provide sample—typically age 16+)
- Symptomatic pain affecting quality of life
Rationale for early treatment: The “catch-up growth” phenomenon—repaired testicles often grow to match the normal side, potentially preserving future fertility. Studies show 70-80% of adolescents with volume asymmetry experience catch-up growth after varicocelectomy.
Monitoring approach: For asymptomatic adolescents with symmetric testicular size:
- Annual physical examination
- Ultrasound every 12-18 months until skeletal maturity
- Semen analysis at age 16-18 if clinically indicated
Men with Recurrent Varicocele
Despite high success rates, varicoceles recur in 1-15% of cases (technique-dependent).
Causes of recurrence:
- Incomplete initial ligation (missed collateral veins)
- Development of new collateral pathways
- Technical factors during initial surgery
Diagnosis: Similar to primary diagnosis—physical exam, Doppler ultrasound showing retrograde flow
Treatment options:
- Repeat microsurgical varicocelectomy: 90-95% success rate for recurrence
- Percutaneous embolization: Often preferred for recurrence (avoids scar tissue from previous surgery)
- Observation: If asymptomatic with stable semen parameters
Outcomes: Second procedures typically achieve similar improvement rates as primary repairs.
Men with Bilateral Varicoceles
Bilateral varicoceles occur in approximately 10% of cases and may have greater fertility impact.
Considerations:
- Higher likelihood of azoospermia or severe oligospermia
- Typically requires bilateral treatment
- Laparoscopic or bilateral microsurgical approach
- Longer operative time but addressed in single procedure
Outcomes: Success rates similar to unilateral repair, with 65-75% showing sperm parameter improvement and 35-45% achieving pregnancy.
Older Men (Age 40+)
Age-related considerations:
- Natural decline in sperm quality accelerates after age 40
- Varicocele repair success rates slightly lower (50-60% improvement vs. 70-80% in younger men)
- Partner age becomes critical factor—female age >35 significantly impacts conception regardless of male fertility
- Faster progression to ART oftenappropriate due to biological clock considerations
- Testosterone benefits: Interestingly, older men may experience additional benefits from varicocele repair beyond fertility. A 2023 study in Andrology found that men aged 40-55 who underwent varicocelectomy experienced:
- Average testosterone increase of 84 ng/dL (from 387 to 471 ng/dL)
- Improved erectile function scores
- Reduced fatigue and improved mood
- Better overall sexual satisfaction
- Decision-making framework for older men:
- If partner is <35 years: Consider varicocelectomy first (6-9 month trial)
- If partner is 35-38 years: Parallel approach—surgery with concurrent fertility evaluation of partner, proceed to ART if no improvement by 6 months
- If partner is >38 years: Often proceed directly to IVF/ICSI while considering surgery for testosterone/symptom benefits
- Men with Azoospermia (Zero Sperm Count)
- Approximately 1% of all men and 10-15% of infertile men have azoospermia.
- Types:
- Obstructive azoospermia (OA): Blockage prevents sperm from reaching ejaculate (sperm production is normal)
- Non-obstructive azoospermia (NOA): Impaired sperm production
- Varicocele and NOA:
- Can varicocele repair help men with zero sperm count? The answer is sometimes yes—but requires careful selection.
- Research evidence: A 2024 meta-analysis of 16 studies examining varicocelectomy in NOA patients found:
- 42% of men had sperm appear in ejaculate post-surgery (conversion to oligospermia)
- Mean time to sperm appearance: 4-8 months post-surgery
- 18% achieved natural pregnancy
- For those remaining azoospermic, sperm retrieval rates during micro-TESE were 1.5x higher than untreated controls
- Best candidates for surgery with NOA:
- Palpable Grade 2-3 varicoceles
- Testicular volume >12 mL
- FSH <15 mIU/mL
- At least one testis with normal consistency
- No genetic abnormalities (normal karyotype, no Y-chromosome microdeletions)
- Clinical pearl: Even if sperm don’t appear in ejaculate, varicocele repair may improve the testicular environment enough to enhance surgical sperm retrieval success for ICSI.
- Understanding Success and Setting Realistic Expectations
- One of the most challenging aspects of varicocele treatment is managing expectations. Not everyone responds the same way, and success means different things to different people.
- Defining Success: Multiple Metrics
- Semen parameter improvement: 60-80% show improvement in at least one parameter Natural pregnancy: 32-43% achieve pregnancy within 12-24 months post-surgery Improved ART outcomes: Even without natural conception, improved sperm quality enhances IVF/ICSI success Testosterone improvement: 70-80% experience increases, especially beneficial for older men Symptom relief: 85-90% experience reduction in pain/discomfort (for symptomatic varicoceles) Testicular growth: 70-80% of adolescents with asymmetry show catch-up growth
- Predictors of Treatment Success
- Factors associated with better outcomes:
- Patient factors:
- Younger age (<35 years)
- Shorter duration of infertility (<3 years)
- No history of cryptorchidism (undescended testicle)
- Normal karyotype and no genetic abnormalities
- Absence of other male factor issues (smoking, obesity, medications)
- Varicocele characteristics:
- Larger grade (Grade 2-3 respond better than Grade 1)
- Unilateral left-sided varicocele
- Significant venous reflux on Doppler ultrasound
- Baseline fertility parameters:
- Sperm concentration >5 million/mL
- Some motile sperm present
- FSH <10 mIU/mL
- Testicular volume >15 mL
- DNA fragmentation index <30%
- Female partner factors:
- Age <35 years
- Regular ovulation
- Normal uterine and tubal anatomy
- No significant female factor infertility
- Surgical factors:
- Microsurgical technique
- Experienced surgeon (>50 cases/year)
- Complete ligation of all varicocele veins
- Preservation of arteries and lymphatics
When Treatment Doesn’t Work: Non-Responders
Approximately 20-30% of men show minimal or no improvement in semen parameters after varicocelectomy.
Possible explanations:
- Irreversible damage: Years of elevated temperature and oxidative stress may have caused permanent testicular injury
- Other contributing factors: Undiagnosed genetic issues, hormonal problems, or lifestyle factors
- Incomplete repair: Persistent or recurrent varicocele
- Primary testicular failure: Varicocele may have been incidental, not causative
What to do if treatment doesn’t work:
- Repeat semen analysis: Wait full 6-9 months for maximum improvement; sometimes delayed responders improve at 12 months
- Post-operative ultrasound: Confirm complete varicocele resolution and no recurrence
- Advanced sperm testing: DNA fragmentation, ROS levels may reveal residual issues
- Hormonal reassessment: Check if testosterone improved even if sperm parameters didn’t
- Comprehensive male fertility evaluation: Look for other contributing factors (genetic testing, specialized hormone panels)
- Female partner evaluation: Rule out female factor issues that may be primary obstacle
- Consider ART: Proceed to IUI/IVF/ICSI based on remaining parameters and couple’s goals
Important message: Lack of semen parameter improvement doesn’t always mean failure—some men still achieve pregnancy through natural conception or see enhanced success with ART due to reduced DNA fragmentation and improved embryo quality.
Real-World Case Studies: Patient Journeys
The following represent composite cases drawn from published literature and clinical experience, illustrating common scenarios and outcomes.
Case Study 1: Young Couple with Primary Infertility
Patient profile:
- Male: 29 years old, otherwise healthy
- Female partner: 27 years old, regular cycles, normal HSG
- Time trying: 18 months
Presentation:
- Grade 2 left varicocele discovered during fertility evaluation
- Occasional dull scrotal discomfort after prolonged standing
- Initial semen analysis:
- Concentration: 12 million/mL
- Motility: 25%
- Morphology: 3% normal forms
- Volume: 3.2 mL
Treatment decision: After counseling, couple chose microsurgical varicocelectomy
- Surgery performed without complications
- Post-operative recovery: 10 days to normal activities
Outcomes:
- 3-month post-op semen analysis: Modest improvement (concentration 18 million/mL, motility 32%)
- 6-month analysis: Continued improvement (concentration 28 million/mL, motility 44%, morphology 5%)
- Month 8 post-surgery: Natural pregnancy achieved
- Healthy baby boy delivered
Key takeaways: Young age, short infertility duration, and no female factors contributed to excellent outcome. Patience during the 6-9 month improvement window was critical.
Case Study 2: Advanced Maternal Age Requiring Parallel Approach
Patient profile:
- Male: 34 years old, Grade 3 left varicocele
- Female partner: 39 years old, diminished ovarian reserve (AMH 0.8 ng/mL)
- Time trying: 24 months
Presentation:
- Initial semen analysis:
- Concentration: 8 million/mL
- Motility: 18%
- DNA fragmentation: 42% (elevated)
Treatment decision:
- Parallel approach: Varicocelectomy performed while simultaneously beginning IVF preparation
- Female partner underwent ovarian stimulation 2 months post-surgery
Outcomes:
- 4-month post-op semen analysis showed improvement (concentration 19 million/mL, motility 31%, DFI 28%)
- IVF with ICSI performed at month 5 post-surgery
- Improved sperm quality resulted in better embryo development: 8 eggs retrieved, 6 fertilized, 4 blastocysts formed (50% blast formation rate, above expected for age)
- PGT-A testing: 2 euploid embryos
- First embryo transfer: Successful pregnancy
- Healthy twins delivered
Key takeaways: Advanced maternal age made time-sensitive approach necessary. Varicocele repair improved embryo quality even though natural conception wasn’t achieved. The couple appreciated having addressed the varicocele for potential future fertility while not losing valuable time.
Case Study 3: Adolescent with Testicular Asymmetry
Patient profile:
- 16-year-old male
- Grade 2 left varicocele discovered during sports physical
- No pain or symptoms
Presentation:
- Testicular volumes: Left 12 mL, Right 20 mL (40% asymmetry)
- No semen analysis performed (patient declined)
- Ultrasound confirmed varicocele with significant reflux
Treatment decision:
- After 12-month observation showing persistent asymmetry and no catch-up growth, microscopic varicocelectomy recommended and performed
Outcomes:
- Surgical recovery: Uneventful, returned to sports at 4 weeks
- 6-month post-op: Left testis measured 16 mL (20% catch-up growth)
- 12-month post-op: Left testis measured 18 mL (90% of right testis)
- 24-month post-op: Volumes essentially equal (left 19 mL, right 20 mL)
- At age 19 (3 years post-surgery): Semen analysis performed showing normal parameters
Key takeaways: Significant asymmetry (>20%) justified intervention despite young age. Excellent catch-up growth preserved future fertility potential. Early intervention likely prevented irreversible testicular damage.
Case Study 4: Non-Responder Who Succeeded with ICSI
Patient profile:
- Male: 36 years old, bilateral Grade 2 varicoceles
- Female partner: 33 years old, normal fertility evaluation
- Time trying: 30 months
Presentation:
- Initial semen analysis:
- Concentration: 4.2 million/mL
- Motility: 12%
- Morphology: 1%
- FSH: 14.8 mIU/mL
Treatment decision:
- Bilateral microsurgical varicocelectomy performed
- Concurrent antioxidant supplementation (CoQ10, L-carnitine, vitamins C & E)
Outcomes:
- 6-month post-op analysis: Minimal improvement (concentration 5.8 million/mL, motility 15%)
- 9-month post-op analysis: Slight further improvement (concentration 7.1 million/mL) but still severely oligoasthenozoospermic
- Decision made to proceed with IVF/ICSI
- DNA fragmentation testing showed improvement from 48% pre-op to 31% post-op (despite minimal count/motility improvement)
- IVF cycle: 12 eggs retrieved, 11 fertilized with ICSI, 8 day-5 blastocysts (high blast formation attributed to improved DNA integrity)
- First embryo transfer: Successful pregnancy
- Healthy daughter delivered
- Two euploid embryos frozen for future family planning
Key takeaways: Not all men are “semen parameter responders,” but other markers (DNA fragmentation) may improve. These improvements can significantly impact ART success. The couple was glad they pursued surgery even though natural conception didn’t occur—their embryo quality was notably better than expected for the sperm parameters.
Case Study 5: Testosterone and Quality of Life Benefits
Patient profile:
- Male: 48 years old, Grade 3 left varicocele
- Completed family (two children, ages 12 and 15)
- Not seeking fertility
Presentation:
- Chief complaint: Chronic scrotal discomfort, especially end of day
- Secondary complaints: Fatigue, reduced libido
- Testosterone: 312 ng/dL (low-normal)
- No interest in semen analysis (vasectomy performed years ago)
Treatment decision:
- Microsurgical varicocelectomy offered primarily for pain relief and potential testosterone improvement
- Patient counseled that testosterone improvement not guaranteed
Outcomes:
- Pain: Completely resolved by 6 weeks post-op
- 3-month post-op testosterone: 428 ng/dL
- 6-month post-op testosterone: 441 ng/dL
- Patient reported: “I feel like I did 10 years ago—more energy, better mood, improved relationship with wife”
- No complications
Key takeaways: Varicocele repair offers benefits beyond fertility. Men with symptomatic varicoceles and/or low testosterone may experience significant quality-of-life improvements regardless of fertility goals.
Myths, Misconceptions, and Frequently Misunderstood Facts
Myth 1: “All varicoceles cause infertility”
Reality: Many men with varicoceles are fertile. Approximately 60-65% of men with varicoceles have normal semen parameters and father children without difficulty. The presence of a varicocele doesn’t automatically mean infertility—it’s a risk factor that interacts with many other variables.
Myth 2: “Grade 1 or subclinical varicoceles don’t matter”
Reality: While larger varicoceles typically have greater impact, Grade 1 and subclinical varicoceles can still affect fertility in some men. The relationship between grade and fertility impact isn’t perfectly linear. Some men with Grade 1 varicoceles have severely impaired semen parameters, while others with Grade 3 varicoceles remain fertile. Individual assessment is essential.
Myth 3: “Surgery guarantees improved fertility”
Reality: Varicocelectomy improves semen parameters in 60-80% of men and leads to pregnancy in 32-43% of couples within 1-2 years. These are significant improvements over untreated varicoceles (16-17% pregnancy rate), but success isn’t guaranteed. Approximately 20-30% of men show minimal response to surgery.
Myth 4: “Varicocele only affects the left testicle”
Reality: While 85-90% occur on the left side due to anatomical factors, bilateral varicoceles occur in ~10% of cases, and right-sided varicoceles occur in 1-2%. Additionally, a unilateral varicocele can affect sperm production from both testicles due to shared hormonal and systemic factors.
Myth 5: “You can ‘exercise away’ a varicocele”
Reality: Exercise and lifestyle modifications cannot eliminate a varicocele. However, they can help manage symptoms and may improve overall fertility by reducing contributing factors like obesity, poor circulation, and oxidative stress. Exercise is complementary, not curative.
Myth 6: “Surgery is always the first choice”
Reality: Conservative management is appropriate for many scenarios: subclinical varicoceles with normal semen parameters, completed families, men awaiting partner fertility evaluation, or situations where surgical risks outweigh benefits. Surgery should be a thoughtful decision based on comprehensive evaluation—not a reflex response to varicocele diagnosis.
Myth 7: “Once treated, varicoceles never come back”
Reality: Recurrence rates vary by technique: 1-2% with microsurgical repair, 5-15% with laparoscopy, 10-15% with open techniques, and 10-15% with embolization. While microsurgery has the lowest recurrence, no technique is 100% permanent. Follow-up is important.
Myth 8: “Varicoceles cause erectile dysfunction”
Reality: Varicoceles don’t directly cause erectile dysfunction (ED). However, they may indirectly contribute through reduced testosterone levels in some men. Additionally, anxiety about fertility can contribute to sexual difficulties. Treating the varicocele and addressing testosterone may help ED symptoms if they’re related, but ED usually has other primary causes.
Myth 9: “You’ll feel it if you have a significant varicocele”
Reality: Many varicoceles—including large Grade 3 varicoceles—are completely asymptomatic. Approximately 35-40% of men with varicoceles experience no pain or discomfort whatsoever. Absence of symptoms doesn’t indicate absence of fertility impact. This is why thorough physical examination is part of every infertility evaluation.
Myth 10: “Varicocele surgery is extremely painful with long recovery”
Reality: Modern microsurgical techniques involve small incisions and careful tissue handling. Most men describe post-operative discomfort as mild to moderate, well-controlled with over-the-counter pain medication. Typical recovery: 7-10 days to normal daily activities, 2-3 weeks to exercise, 3-4 weeks to strenuous activities. Most men are pleasantly surprised by how manageable recovery is.
Comprehensive FAQ: Expert Answers to Common Questions
Q1: How long after varicocele surgery before we can try to conceive?
Answer: Most reproductive urologists recommend waiting at least 3 months after surgery before actively trying to conceive, with optimal timing being 6-9 months post-surgery.
Here’s why: Sperm take approximately 72 days (2.5 months) to mature from initial germ cells to fully developed spermatozoa. However, maximum improvement typically occurs at 6-9 months post-surgery because:
- Initial sperm cycles post-surgery may still reflect pre-surgical conditions
- The testicular environment needs time to fully recover from heat and oxidative stress
- Hormonal adjustments occur gradually
That said, there’s no medical reason to avoid trying earlier if you choose—some couples conceive at 3-4 months. The 6-9 month recommendation simply represents the timeframe when success rates are highest. Consider having a follow-up semen analysis at 3 months and again at 6 months to track improvement and adjust your approach accordingly.
Q2: Can a varicocele develop suddenly, or is it something you’re born with?
Answer: Both scenarios can occur, though most varicoceles develop during puberty rather than being present from birth.
Developmental varicoceles: Most varicoceles form during adolescence (ages 11-16) as rapid testicular growth increases blood flow demands. The valves in testicular veins may become incompetent as the vascular system adapts to increased flow volume. Once formed, varicoceles typically persist unless treated—they rarely resolve spontaneously.
Adult-onset varicoceles: While less common, varicoceles can develop in adulthood due to:
- Increased intra-abdominal pressure from weight gain
- Occupational factors (heavy lifting, prolonged standing)
- Obstruction of venous drainage from abdominal masses or kidney tumors (especially with isolated right-sided varicoceles)
Clinical pearl: A varicocele that appears suddenly in a man over 40, particularly on the right side, warrants imaging (CT or MRI) of the abdomen and pelvis to rule out obstruction from tumor or other pathology.
Q3: If my semen analysis is normal, do I still need to treat my varicocele?
Answer: This is highly individualized. If you have a palpable varicocele but normal semen parameters, current fertility, and no symptoms, treatment is generally not indicated.
Consider observation if:
- Semen analysis shows all parameters within normal range
- No pain or discomfort
- Partner is conceiving or has conceived
- No testicular atrophy or asymmetry
Consider treatment if:
- Planning for future fertility and want to protect long-term sperm production
- Experiencing pain or discomfort affecting quality of life
- Testosterone is low or declining
- Testicular asymmetry is present (especially in adolescents)
- Couple is having difficulty conceiving despite “normal” semen analysis (some parameters may be low-normal)
Important nuance: “Normal” semen analysis doesn’t guarantee optimal fertility. Some men with parameters in the normal range but on the lower end may benefit from varicocele treatment to optimize conception chances, particularly if female partner is over 35 or other mild fertility factors exist.
Q4: Can varicoceles cause complete infertility, or can you always have some level of fertility?
Answer: Varicoceles rarely cause complete infertility (azoospermia—zero sperm), but they can severely impair fertility to the point where natural conception is extremely unlikely without intervention.
Spectrum of impact:
- Mild impact: Slight reduction in parameters, natural conception occurs with slightly longer time to pregnancy
- Moderate impact: Significant parameter reduction, natural conception possible but may require 1-2+ years
- Severe impact: Profound oligospermia (<5 million/mL) or severe asthenozoospermia (<5% motility), natural conception unlikely, ART typically required
- Complete azoospermia: Occurs in approximately 5-10% of varicocele cases with non-obstructive azoospermia
Even men with very poor parameters due to varicoceles typically have some sperm production—surgical retrieval combined with ICSI can often achieve pregnancy even when ejaculated sperm are absent or of extremely poor quality.
Q5: Are there any risks to NOT treating a varicocele if I don’t want children?
Answer: If you’ve completed your family or don’t desire children, untreated varicocele carries minimal risk—with a few caveats:
Potential considerations:
- Testosterone decline: Some evidence suggests untreated varicoceles may contribute to more rapid age-related testosterone decline, potentially affecting energy, libido, muscle mass, and mood in later decades
- Testicular atrophy: Progressive atrophy can occur, though this doesn’t affect men who aren’t concerned about fertility
- Chronic discomfort: Approximately 2-4% of initially asymptomatic varicoceles become symptomatic over time
- Changing life circumstances: Some men later regret not addressing varicocele when considering second families or new relationships
Bottom line: There’s no medical urgency to treat asymptomatic varicoceles when fertility isn’t desired. However, if you’re experiencing pain, declining testosterone symptoms, or want to preserve the option of future fertility, treatment merits consideration.
Q6: How do I find an experienced microsurgeon for varicocele repair?
Answer: Finding a skilled surgeon significantly impacts outcomes. Here’s how to identify qualified specialists:
Look for:
- Board-certified urologist with fellowship training in male infertility/andrology
- High surgical volume: Surgeons performing 50+ microsurgical varicocelectomies annually have superior outcomes
- Academic or specialized practice: Urologists at academic medical centers or specialized fertility centers typically have more experience
- Publications and research: Surgeons contributing to varicocele literature demonstrate expertise
Questions to ask:
- How many microsurgical varicocelectomies do you perform annually?
- What are your success rates for semen parameter improvement?
- What’s your recurrence rate?
- What’s your hydrocele formation rate?
- Do you use an operating microscope or loupes?
- What’s your approach to preserving lymphatics and arteries?
Red flags:
- Urologist primarily does other procedures (prostate, stones, cancer) with occasional varicocele repair
- Use of older techniques (non-microsurgical open repair) without clear rationale
- Unwilling to discuss complication and success rates
Resources:
- American Society for Reproductive Medicine (ASRM) physician directory
- Society for Male Reproduction and Urology (SMRU) member list
- Academic medical center urology departments
- Fertility clinic referrals
Future Directions: Emerging Research and Novel Approaches
The field of varicocele management and male fertility continues to evolve. Here are areas of active investigation:
Biomarkers for Treatment Response
Researchers are working to identify markers that predict which men will respond to varicocele repair:
- Sperm DNA fragmentation index: Men with DFI >30% may benefit most from surgery
- Seminal oxidative stress markers: ROS levels and antioxidant capacity may predict response
- MicroRNAs: Small RNA molecules in seminal plasma showing promise as predictive biomarkers
- Advanced imaging: Elastography and contrast-enhanced ultrasound to assess testicular tissue quality
The goal: personalized treatment decisions based on objective biological markers rather than population statistics.
Novel Surgical Techniques
Robotic-assisted varicocelectomy: Early studies of robot-assisted microsurgical repair show:
- Similar outcomes to conventional microsurgery
- Potentially shorter learning curve for surgeons
- Enhanced 3D visualization
- Current limitation: Higher cost, limited availability
Lymphatic mapping techniques: Using indocyanine green fluorescence to identify and preserve lymphatic channels during surgery may further reduce hydrocele risk.
Advanced Sperm Selection for ART
For men with persistent poor semen quality post-varicocelectomy:
- Physiologic ICSI (PICSI): Uses hyaluronic acid binding to select mature sperm with better DNA integrity
- Microfluidic sperm sorting: Lab-on-chip devices that select sperm based on swimming ability and morphology
- Magnetic-activated cell sorting (MACS): Removes apoptotic (dying) sperm from samples
- Zeta potential selection: Separates sperm based on surface electrical charge
These technologies aim to identify the healthiest sperm from poor-quality samples, potentially improving ICSI outcomes.
Pharmacological Interventions
Anti-inflammatory medications: Some research suggests specific anti-inflammatory agents may reduce oxidative damage from varicoceles:
- Pentoxifylline: Improves sperm motility in preliminary studies
- Antioxidant combinations: Optimized formulations based on oxidative stress profiles
Hormonal modulation: Selective estrogen receptor modulators (SERMs) like clomiphene citrate are being studied as adjuncts to surgery to optimize testosterone and sperm production.
Regenerative Medicine Approaches
Stem cell therapy: Very preliminary research (mostly animal models) is exploring whether stem cell treatments could regenerate damaged testicular tissue in severe cases. This remains highly experimental with no human applications yet.
Platelet-rich plasma (PRP): Some centers are investigating intratesticular PRP injection following varicocele repair to potentially enhance tissue healing and regeneration. This is considered experimental and not standard of care.
Taking Action: Your Next Steps
If you’re dealing with a varicocele and fertility concerns, here’s a practical roadmap:
Step 1: Comprehensive Evaluation (Weeks 1-4)
- Physical examination by urologist or reproductive specialist
- Semen analysis (2 samples, 2-4 weeks apart)
- Scrotal ultrasound if clinical findings are unclear or subclinical varicocele suspected
- Hormonal testing: FSH, LH, total testosterone (morning sample), estradiol
- Partner fertility evaluation: Ensure comprehensive assessment of both partners
Step 2: Review Results and Discuss Options (Week 4-6)
- Discuss findings with reproductive urologist
- Consider fertility specialist consultation for couple-based treatment planning
- Weigh treatment options: surgery vs. observation vs. ART vs. combined approaches
- Factor in timeline pressures (maternal age, personal circumstances)
- Consider second opinion if diagnosis or treatment recommendations are unclear
Step 3: Implement Initial Management (Months 1-3)
If choosing surgery:
- Schedule microsurgical varicocelectomy
- Post-operative recovery and follow-up
- Begin or continue antioxidant supplementation
- Implement lifestyle modifications
If choosing observation:
- Optimize lifestyle factors immediately (weight management, temperature avoidance, diet, supplements)
- Consider supportive underwear for symptom relief
- Schedule follow-up semen analysis in 3-6 months
- Begin trying to conceive naturally (if not already)
If choosing ART:
- Complete fertility workup for partner
- Consider varicocele repair as adjunct to improve outcomes
- Schedule with reproductive endocrinologist
Step 4: Monitor and Adjust (Months 3-12)
- Post-surgical patients: Semen analysis at 3, 6, and potentially 9 months
- Observation patients: Semen analysis every 3-6 months to track changes
- All patients: Continue lifestyle optimization and supplementation
- Adjust plan based on results—remain flexible and evidence-guided
Step 5: Evaluate Outcomes and Next Steps (Month 12+)
- If pregnancy achieved: Success! Consider varicocele management for future fertility
- If semen improved but no pregnancy: Continue trying or consider IUI
- If minimal response to treatment: Reassess with advanced testing, consider ART
- If female factor identified: Address both partners’ issues simultaneously
Conclusion: Knowledge, Hope, and Realistic Optimism
A varicocele diagnosis can feel overwhelming—especially when you’re hoping to start or grow your family. The uncertainty about fertility, the medical terminology, the treatment decisions—it’s a lot to process.
Here’s what I want you to remember:
You’re not alone. Varicoceles affect millions of men worldwide. It’s one of the most common and treatable causes of male infertility. The medical community has decades of research and experience helping men in your exact situation.
Knowledge is power. Understanding the connection between varicoceles and fertility, the mechanisms of damage, and the evidence behind treatments empowers you to make informed decisions aligned with your values and goals.
Treatment works for most men. While success isn’t guaranteed, 60-80% of men experience improved semen parameters after varicocele repair, and 32-43% of couples achieve pregnancy naturally within 1-2 years—substantially better than untreated varicoceles. Even non-responders often benefit from improved ART outcomes.
Multiple pathways exist. If one approach doesn’t work, others are available. Modern reproductive medicine offers numerous solutions—from surgery to lifestyle optimization to assisted reproduction. One way or another, most couples determined to have children find a path forward.
Time matters—but don’t panic. While earlier intervention generally produces better results, varicocele isn’t an emergency. Take time to complete thorough evaluations, consider your options, and make thoughtful decisions. Rushed decisions rarely lead to better outcomes.
Your overall health matters too. Varicocele treatment offers potential benefits beyond fertility—improved testosterone, reduced discomfort, and preserved long-term reproductive health. These considerations remain important even if immediate fertility isn’t your primary concern.
Stay engaged and advocate for yourself. Ask questions, seek explanations, request data on success rates, and don’t hesitate to get second opinions. Your fertility journey is deeply personal—ensure you have confidence in your medical team and treatment plan.
The path from varicocele diagnosis to parenthood isn’t always straightforward, but it’s traveled successfully by hundreds of thousands of men each year. With proper evaluation, evidence-based treatment, realistic expectations, and persistence, most men with varicocele-related fertility challenges ultimately achieve their family-building goals.
Your journey begins with information—and you’ve taken that crucial first step.
Last Updated: November 2025
Medical Disclaimer: This article provides general information about varicoceles and fertility. Individual situations vary significantly—always consult qualified healthcare professionals for diagnosis and personalized treatment recommendations. Treatment decisions should be made based on comprehensive evaluation of both partners and individual circumstances.