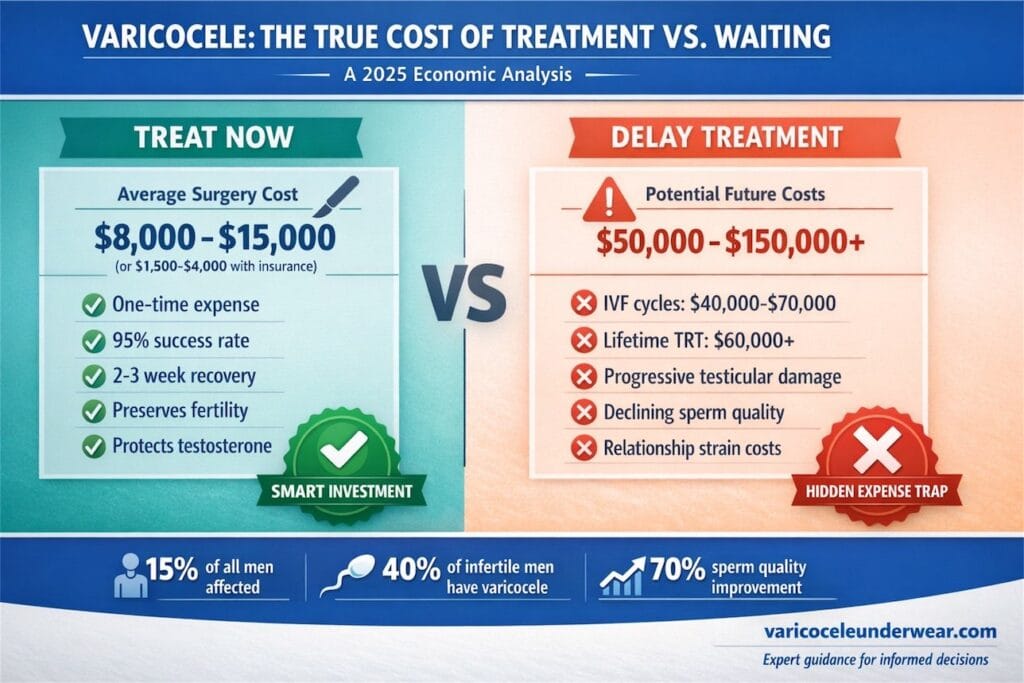
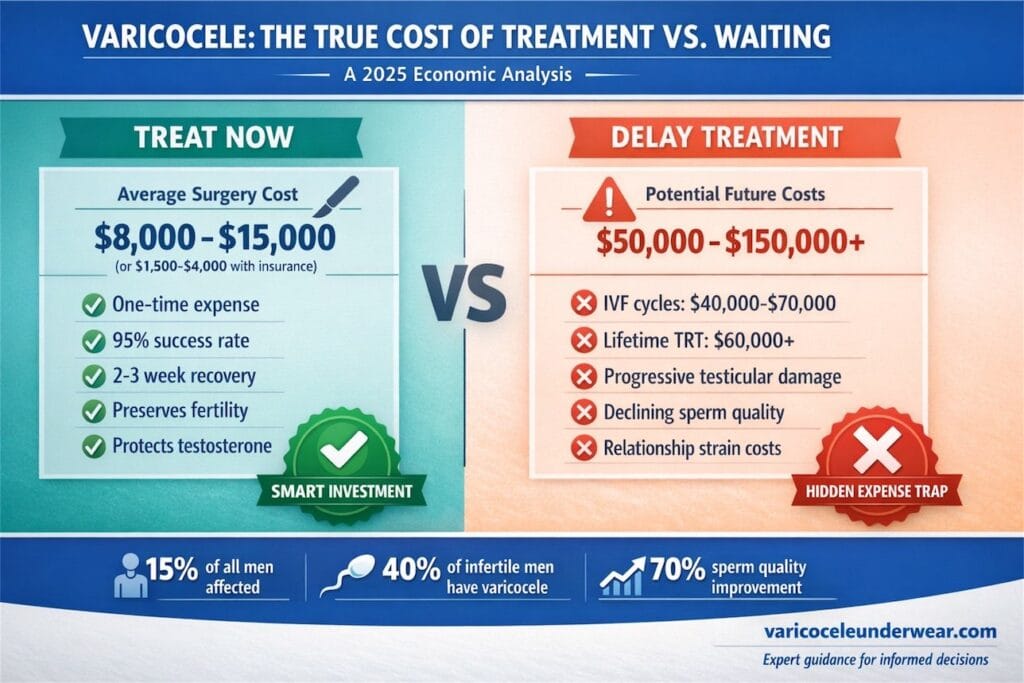
If you have been diagnosed with varicocele, you are likely weighing a difficult question: Should I pay for treatment now, or wait and see? This decision affects roughly 15% of all men and up to 40% of those experiencing infertility. The financial stakes are real, and the health consequences of waiting can multiply costs significantly over time.
This article breaks down the true economics of varicocele management. You will learn actual treatment costs, insurance realities, and the often-overlooked expenses of delayed care. We also examine how conservative approaches, including supportive underwear and lifestyle modifications, fit into a cost-effective management strategy.
For comprehensive information about all available treatment options, our complete varicocele treatment guide covers everything from watchful waiting to surgical intervention.
How Much Does Varicocele Treatment Cost in 2026?
Treatment costs vary widely based on the procedure type, geographic location, facility choice, and insurance status. Here is a current breakdown based on 2026 healthcare pricing data.
Surgical and Procedural Cost Comparison Table
| Treatment Type | Average Cost (Uninsured) | Average Cost (With Insurance) | Recovery Time |
|---|---|---|---|
| Microsurgical Varicocelectomy | $8,000 – $15,000 | $1,500 – $4,000 | 2-3 weeks |
| Laparoscopic Varicocelectomy | $10,000 – $18,000 | $2,000 – $5,000 | 1-2 weeks |
| Percutaneous Embolization | $5,000 – $12,000 | $1,000 – $3,500 | 1-2 days |
| Open Inguinal Surgery | $6,000 – $12,000 | $1,200 – $3,500 | 2-4 weeks |
These figures include surgeon fees, anesthesia, facility charges, and basic follow-up care. They do not include pre-operative testing, which typically adds $300 to $800, or potential complication management.
What Factors Affect Your Final Bill?
Several variables influence your out-of-pocket expenses:
Geographic location matters significantly. Urban centers and coastal regions typically charge 20-40% more than rural or Midwestern facilities. A microsurgical repair in Manhattan might cost $18,000, while the same procedure in Ohio could be $9,000.
Facility type changes pricing dramatically. Ambulatory surgery centers often charge 40-60% less than hospital-based operating rooms for identical procedures. Ask your surgeon about outpatient options.
Surgeon experience affects both cost and outcomes. High-volume specialists may charge premium fees but typically deliver lower complication rates. This often translates to better long-term value despite higher upfront costs.
Does Insurance Cover Varicocele Surgery?
Insurance coverage for varicocele treatment remains inconsistent across carriers and plan types. Understanding your policy specifics is essential before scheduling any procedure.
When Insurance Typically Approves Coverage
Most insurance plans cover varicocele surgery when documented medical necessity exists. Approval criteria generally include:
- Chronic testicular pain lasting more than 3 months
- Documented infertility with abnormal semen analysis
- Testicular atrophy (shrinkage) confirmed by ultrasound
- Failed conservative management attempts
According to the American Urological Association guidelines, treatment is recommended for men with palpable varicocele, documented infertility, and abnormal semen parameters when the female partner has normal fertility or correctable issues.
Common Insurance Denial Reasons
Insurance companies frequently deny coverage for:
- Subclinical varicoceles (detectable only by ultrasound)
- Absence of documented symptoms
- Treatment sought primarily for fertility without other medical indications
- Missing documentation of conservative treatment attempts
Pro tip: Request a pre-authorization before scheduling surgery. If denied, ask your urologist for a letter of medical necessity citing peer-reviewed studies on varicocele-related testicular dysfunction.
What Are the Long-Term Health Costs of Untreated Varicocele?
Here is where the economics become complex. Delaying treatment does not eliminate costs. It often transfers them to future healthcare expenses, fertility treatments, and quality-of-life impacts.
Progressive Testicular Damage and Testosterone Decline
Research published in Fertility and Sterility demonstrates that untreated varicoceles cause progressive testicular dysfunction over time. This damage manifests in several expensive ways:
Testosterone replacement therapy (TRT) costs: Men with varicocele-related hypogonadism may require lifelong testosterone supplementation. Annual TRT costs range from $1,800 to $6,000 depending on delivery method and insurance coverage. Over 20 years, this totals $36,000 to $120,000.
Fertility treatment expenses: Untreated varicocele contributes to declining sperm quality. When couples eventually seek fertility assistance, they face:
| Fertility Treatment | Average Cost Per Cycle | Success Rate |
|---|---|---|
| Intrauterine Insemination (IUI) | $500 – $2,000 | 10-20% |
| In Vitro Fertilization (IVF) | $12,000 – $20,000 | 40-50% |
| IVF with ICSI | $15,000 – $25,000 | 50-60% |
| Sperm Retrieval (TESE) | $5,000 – $10,000 | Variable |
Most couples require multiple cycles. The average IVF patient undergoes 2.7 cycles before success or discontinuation, pushing total costs toward $40,000 to $70,000.
The ROI of Early Treatment
A 2023 cost-effectiveness analysis compared varicocele repair against proceeding directly to assisted reproduction. The findings were clear: microsurgical varicocelectomy delivered superior cost-per-live-birth outcomes for most couples.
Case study: Michael, 29, presented with grade 2 varicocele and borderline semen parameters. His options:
- Option A: Immediate microsurgical repair ($3,200 after insurance) plus 12 months of natural conception attempts
- Option B: Skip surgery, proceed to IVF after 6 months ($38,000 for two cycles)
Michael chose Option A. His sperm concentration improved from 8 million to 22 million per milliliter within 6 months. His wife conceived naturally 9 months post-surgery. Total cost: $3,200 plus routine prenatal care.
Conservative Management: Cost-Effective Alternatives to Surgery
Not every varicocele requires surgical intervention. For men with mild symptoms, grade 1 varicoceles, or those not currently pursuing fertility, conservative approaches offer meaningful symptom relief at fraction of surgical costs.
What Does Non-Surgical Management Cost?
Conservative management expenses are minimal compared to procedural interventions:
| Conservative Option | Initial Cost | Annual Cost | Effectiveness |
|---|---|---|---|
| Scrotal Support Underwear | $30 – $80 | $60 – $160 | Symptom relief in 60-70% |
| OTC Pain Management | $10 – $30/month | $120 – $360 | Variable |
| Lifestyle Modifications | $0 | $0 | Supportive |
| Supplements (antioxidants) | $20 – $50/month | $240 – $600 | Modest evidence |
Specialized varicocele support underwear with cooling technology provides targeted compression and temperature regulation. Many men report significant symptom improvement, particularly for activity-related discomfort.
When Is Conservative Management Appropriate?
Conservative approaches work best for:
- Mild, intermittent symptoms
- Men not currently seeking fertility
- Subclinical or grade 1 varicoceles
- Patients awaiting surgery
- Those with contraindications to anesthesia
However, conservative management requires ongoing monitoring. Annual ultrasound evaluation ($200-$500) helps track testicular size and detect progressive damage before it becomes irreversible.
How Do Varicocele Costs Vary by Age and Life Stage?
The economic calculus shifts based on your age, family planning goals, and current symptoms. Here is a life-stage breakdown:
Young Men (18-25): Prevention-Focused Economics
Adolescents and young adults with varicocele face a critical decision window. Research from the National Institutes of Health indicates that early intervention in younger males preserves testicular function and future fertility potential more effectively than delayed treatment.
Cost consideration: Early repair ($8,000-$15,000 or insurance equivalent) versus potential future fertility treatments ($40,000-$100,000+) plus possible testosterone replacement ($50,000+ lifetime).
Men 25-35: Family Planning Economics
This demographic faces the highest stakes. Fertility preservation directly impacts family-building costs. Every year of delay potentially reduces natural conception probability while increasing reliance on assisted reproduction.
Strategic approach: Obtain baseline semen analysis ($150-$300). If parameters are abnormal, pursue repair before active conception attempts. The math favors surgical intervention for this group.
Men 35+: Symptom and Testosterone Focus
Older men often present with symptomatic varicocele. Pain, heaviness, and testicular atrophy drive treatment decisions more than fertility concerns. Untreated varicocele correlates with accelerated testosterone decline, creating downstream costs.
Hidden Costs Most Patients Overlook
Beyond direct medical expenses, varicocele creates indirect economic impacts that rarely appear in cost comparisons.
Lost Productivity and Income
Surgical recovery requires 1-3 weeks away from physically demanding work. For hourly workers without paid leave, this translates to:
- 1-week recovery: $500-$1,500 lost wages
- 3-week recovery: $1,500-$4,500 lost wages
- Complications extending recovery: $3,000+ additional losses
Relationship and Mental Health Costs
Infertility strains relationships. Couples experiencing fertility challenges report:
- 40% higher divorce rates than fertile couples
- Increased rates of depression and anxiety
- Marriage counseling costs ($100-$300 per session)
These soft costs rarely factor into treatment decisions but significantly impact total life economics.
Travel and Logistics Expenses
High-volume varicocele surgeons often practice at specialty centers requiring travel. Patients seeking optimal outcomes may incur:
- Airfare or long-distance driving: $200-$800
- Hotel stays: $150-$400
- Companion travel expenses: $200-$600
- Childcare during treatment: $100-$500
Making the Right Financial Decision: A Framework
Approaching varicocele treatment as a financial decision requires balancing immediate costs against probability-weighted future expenses.
Decision Matrix Based on Clinical Factors
| Your Situation | Recommended Approach | Financial Rationale |
|---|---|---|
| Grade 2-3, wanting children within 2 years | Surgical repair | Highest ROI, avoids fertility treatment costs |
| Grade 1, no symptoms, not seeking fertility | Conservative management + monitoring | Low immediate cost, acceptable risk |
| Any grade with chronic pain | Surgical repair | Quality of life improvement, prevent disability |
| Grade 2-3 with testosterone symptoms | Surgical repair | Prevents lifelong TRT costs |
| Any grade, completed family, minimal symptoms | Watchful waiting | Low-cost monitoring appropriate |
Questions to Ask Your Urologist About Costs
Before any treatment decision, get specific answers:
- What is your total fee including follow-up visits?
- What facility charges should I expect?
- What is your complication rate, and what are retreatment costs?
- Do you offer cash-pay discounts?
- Can this be performed at an ambulatory center rather than hospital?
Frequently Asked Questions
Is varicocele surgery worth the cost if I do not want children?
Fertility is only one factor. Varicocele repair also addresses chronic pain, prevents progressive testicular atrophy, and may protect long-term testosterone production. Men with symptomatic varicocele often report significant quality-of-life improvements following repair. The Mayo Clinic notes that pain relief is a valid treatment indication regardless of fertility goals.
Can I negotiate varicocele surgery costs with my provider?
Yes. Cash-pay patients often receive 20-40% discounts when paying upfront. Request itemized estimates and compare prices across facilities. Ambulatory surgery centers typically offer better pricing than hospitals for identical procedures. Some surgeons offer payment plans or accept healthcare credit.
How much money does varicocele repair save on fertility treatments?
Studies indicate varicocele repair is cost-effective compared to proceeding directly to IVF. For couples where the male partner has surgically correctable varicocele, repair plus natural conception attempts costs approximately $10,000-$15,000 less than IVF while achieving comparable pregnancy rates. This savings multiplies if multiple IVF cycles would be required.
Your Next Step: Make an Informed Decision
The economics of varicocele treatment favor early intervention for most men, particularly those planning families or experiencing progressive symptoms. Delaying treatment rarely saves money. It typically shifts costs toward more expensive future interventions while risking permanent testicular damage.
Start with a urological evaluation and baseline semen analysis if fertility matters to you. Get specific cost estimates from multiple providers. Check your insurance benefits before scheduling.
For ongoing symptom management while you evaluate options, specialized support underwear offers affordable, non-invasive relief that many men find helpful.
What financial concerns are influencing your treatment decision? Share your experience in the comments below, or explore our complete varicocele treatment guide for detailed information about all available options.
This article was reviewed for medical accuracy and reflects current clinical guidelines and 2026 healthcare pricing. Individual costs vary by location, insurance, and provider. Consult a board-certified urologist for personalized treatment recommendations.