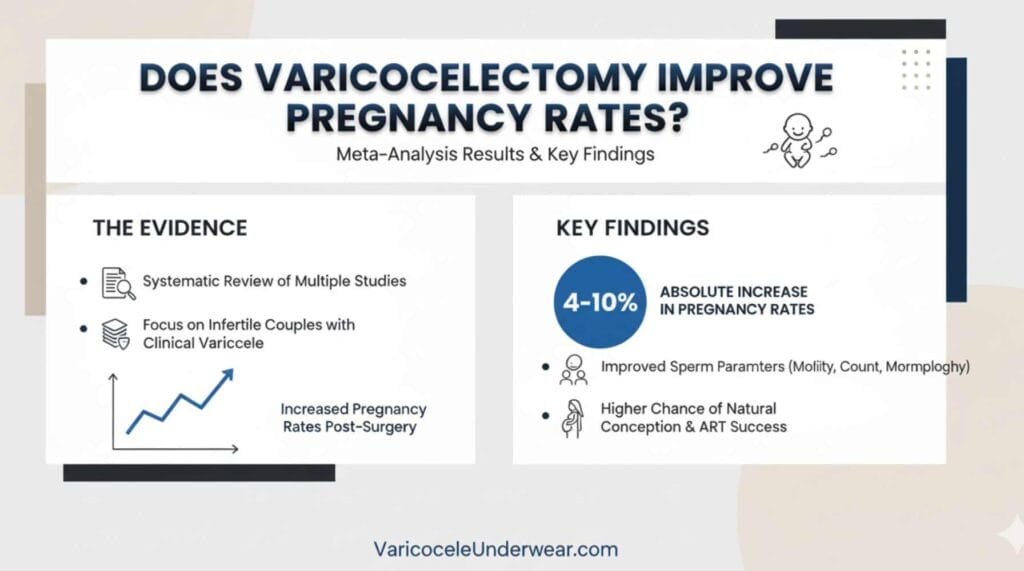
If you’re wondering whether varicocele surgery actually improves your chances of becoming a father, recent meta-analyses provide clear answers. Studies published in 2025 show that varicocelectomy increases clinical pregnancy rates by 38% compared to men who don’t undergo the procedure. For couples dealing with infertility where varicocele is a factor, this surgery represents one of the few correctable causes of male reproductive problems.
Understanding how varicocele affects fertility helps frame why surgical intervention often becomes necessary. The condition damages sperm production through increased testicular temperature and oxidative stress. This article examines what multiple meta-analyses reveal about pregnancy outcomes after varicocele repair, when you can expect results, and what factors predict success.
While waiting for surgery or during recovery, many men find relief using specialized support underwear designed for varicocele that provides cooling and elevation to reduce discomfort.
What Do Recent Meta-Analyses Say About Pregnancy Rates?
A 2025 systematic review analyzing 1,705 infertile men found that varicocelectomy significantly improved clinical pregnancy rates with an odds ratio of 1.38. This means men who had the surgery were 38% more likely to achieve pregnancy compared to those who didn’t undergo treatment. The effect was even stronger in prospective studies, showing an odds ratio of 1.79.
Another comprehensive meta-analysis of 1,357 patients demonstrated that varicocele treatment improved pregnancy rates with an odds ratio of 1.29 and simultaneously increased sperm concentration by an average of 12.34 million sperm per milliliter. These improvements occurred across all grades of varicocele, not just severe cases.
Real-world clinical data supports these findings. A study of 170 men who underwent microscopic varicocelectomy reported an overall pregnancy rate of 40.7% within the follow-up period. Men whose total progressive sperm count improved after surgery had 5.89 times higher odds of achieving pregnancy compared to those who didn’t see improvement.
How Long Before You See Results After Surgery?
Patience matters after varicocelectomy because sperm production follows a 72-day cycle. Most improvements in sperm parameters occur after 3 months post-surgery, with 78.8% of men who showed improvement experiencing it during this timeframe. Some men see changes earlier, but waiting a full 3 to 6 months provides the most accurate assessment.
Pregnancy timing varies:
- 32.3% of couples achieve spontaneous pregnancy after varicocelectomy
- 25.2% succeed through assisted reproductive technologies
- Spontaneous pregnancy rates range from 32% to 41% within one year of surgery
The timeframe doesn’t significantly affect your chances. Whether sperm parameters improve early or late after surgery, pregnancy rates remain similar as long as improvement occurs.
Which Sperm Parameters Improve Most?
Varicocelectomy creates measurable changes in semen analysis:
Sperm concentration: Increases by an average of 12.34 million/ml after surgery
Motility improvements: Both total motility and progressive motility show significant gains, though the magnitude varies between studies
Total progressive sperm count: 69.4% of men experience meaningful improvement in this critical metric
Morphology: Changes in sperm shape and structure show less consistent improvement compared to count and motility
Interestingly, hormone levels typically don’t change significantly after varicocelectomy. The benefits come from improved testicular function rather than hormonal shifts.
Does Varicocele Grade Matter for Success?
Grade 3 varicoceles (the largest, most visible type) show the most dramatic improvements after surgery. These cases demonstrate significant increases in sperm motility, concentration, and testicular volume compared to Grade 1 and Grade 2 varicoceles. However, this doesn’t mean smaller varicoceles shouldn’t be treated.
Studies included all grades of clinical varicoceles and found benefits across the spectrum. The key factor isn’t varicocele size alone but rather the presence of:
- Abnormal semen parameters
- Palpable varicocele on physical exam
- Documented infertility with female partner evaluated
- Testicular size discrepancy
Even bilateral varicocelectomy (18.2% of cases) and redo surgery after recurrence show positive outcomes, with redo procedures achieving a 34.6% pregnancy rate.
What About Assisted Reproduction After Surgery?
Men planning to use IVF or IUI may still benefit from varicocelectomy before attempting assisted reproductive technologies. The 2025 meta-analysis specifically examined ART outcomes and found improved clinical pregnancy rates in men who underwent surgery first.
Surgery before ART offers several advantages:
- Better quality sperm for collection
- Potentially lower need for advanced techniques like ICSI
- Option to attempt natural conception first
- Cost savings if spontaneous pregnancy occurs
However, timing matters. Surgery performed between 2012 and 2019 showed stronger effects (OR: 1.59) compared to earlier or later time periods, possibly reflecting improved surgical techniques and patient selection criteria.
FAQ
How successful is varicocelectomy for getting pregnant naturally?
Spontaneous pregnancy rates after varicocelectomy range from 32% to 41% within one year of surgery. Men whose sperm count improves after the procedure have nearly 6 times higher odds of achieving pregnancy compared to those who don’t see improvement in semen parameters.
Can varicocele surgery improve fertility if my sperm count is very low?
Yes, even men with severely impaired semen parameters can benefit. Surgery increases sperm concentration by an average of 12.34 million sperm per milliliter. The key is whether you achieve improvement after surgery—those who do have significantly better pregnancy outcomes regardless of starting baseline.
Should I have varicocele surgery before trying IVF or IUI?
Meta-analyses show that men who undergo varicocelectomy before assisted reproductive technologies have 38% higher clinical pregnancy rates compared to those who skip surgery. The procedure may improve sperm quality enough to use less invasive fertility treatments or attempt natural conception first.