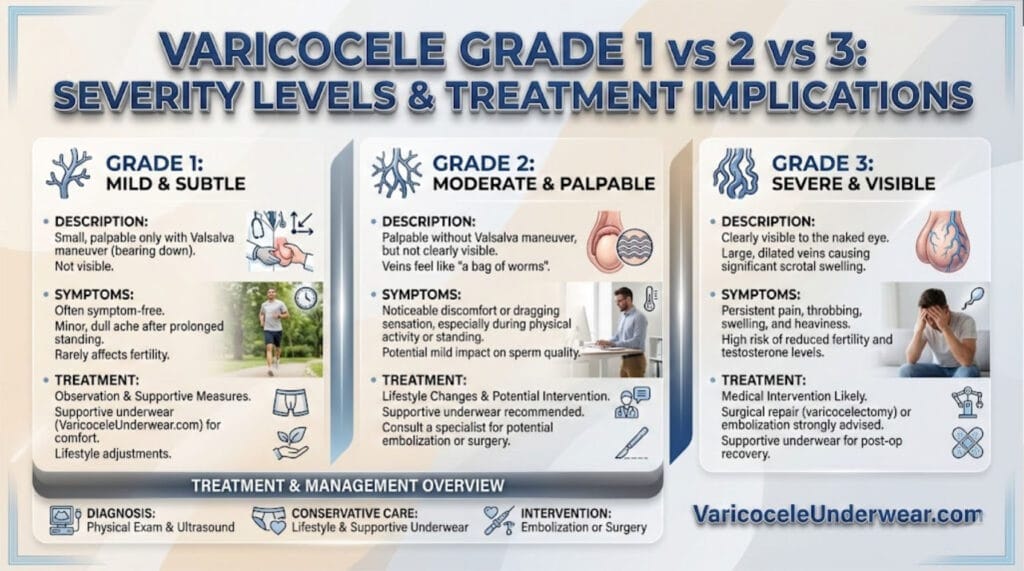
Varicocele grading determines your treatment path. Men with Grade 1 may need observation only, Grade 2 often requires monitoring with possible intervention, and Grade 3 typically needs surgical correction to prevent fertility problems and testicular damage.
Understanding which grade you have matters because each severity level carries different risks for sperm quality, testosterone production, and long-term testicular health. This guide breaks down what separates each grade, how doctors diagnose them, and which treatment options work best for your specific situation. For comprehensive background information, read our complete varicocele guide.
How Doctors Grade Varicoceles
Urologists use a three-tier clinical grading system based on physical examination findings. The classification depends on whether enlarged scrotal veins are visible to the eye, palpable (felt) during examination, or only detectable during specific maneuvers.
Grade 1 varicoceles are the smallest type. A doctor can only feel these enlarged veins when you perform a Valsalva maneuver—bearing down as if having a bowel movement while standing. Without this increased abdominal pressure, Grade 1 varicoceles remain undetectable during routine physical examination.
Grade 2 varicoceles represent moderate severity. These dilated veins are palpable when you’re standing, even without straining or special maneuvers. A urologist can easily feel the enlarged veins during a standard scrotal examination.
Grade 3 varicoceles are the most severe form. These are visible through the scrotal skin without any examination technique required. The scrotum often appears enlarged or asymmetric, and the veins look like a “bag of worms” above the testicle.
A fourth category exists—subclinical varicoceles—which are only detectable through ultrasound imaging and not palpable during physical examination. Current medical guidelines do not recommend treating subclinical varicoceles.
Grade-Specific Impact on Fertility and Testosterone
The grade of your varicocele directly correlates with fertility risks, though even Grade 1 can affect sperm production.
Fertility Effects by Grade
Grade 1 varicoceles generally cause minimal fertility impact but may still produce subtle changes in sperm parameters. Some men with Grade 1 varicoceles show reduced sperm count, decreased motility, or slight morphology abnormalities.
Grade 2 varicoceles create more significant sperm parameter changes. Men at this severity level commonly experience lower sperm concentration, reduced forward movement, and higher percentages of abnormally shaped sperm. These factors make natural conception more challenging.
Grade 3 varicoceles carry the highest fertility risk. This severity level frequently causes oligospermia (low sperm count), asthenospermia (poor sperm motility), and teratospermia (abnormal sperm shape). Grade 3 varicoceles can also lead to testicular atrophy—actual shrinkage of the affected testicle.
Testosterone and Hormonal Effects
Varicoceles affect testosterone production in men across all grades, though the relationship between grade and testosterone levels remains complex. The condition impairs Leydig cell function in both testicles, reducing testosterone secretion and disrupting the hormonal environment needed for healthy sperm production.
Microsurgical varicocele repair increases serum testosterone levels regardless of the initial grade. Men who undergo varicocelectomy typically see testosterone improvements whether they started with Grade 2 or Grade 3 varicoceles.
When Each Grade Needs Treatment
Treatment recommendations depend on your symptoms, fertility goals, and specific grade classification.
Observation vs. Intervention
Current European and American guidelines recommend varicocele treatment for clinically palpable varicoceles (Grade 2 or 3) when you have abnormal semen parameters, unexplained infertility, and your female partner has preserved ovarian reserve.
Grade 1 treatment approach: Most urologists recommend watchful waiting for Grade 1 varicoceles unless you have documented fertility issues or persistent pain. Conservative management includes lifestyle modifications and supportive measures.
Grade 2 treatment considerations: This grade sits in a gray zone. If you have normal sperm parameters and no symptoms, observation may suffice. However, if you’re experiencing fertility problems or discomfort, surgical intervention becomes more appropriate.
Grade 3 treatment protocol: Grade 3 varicoceles typically require surgical correction due to high fertility impairment risk and potential for progressive testicular damage. Waiting rarely benefits men with this severity level.
Conservative Management Options
For mild symptoms across any grade, non-surgical approaches provide relief. Supportive underwear designed for varicocele can reduce discomfort by minimizing scrotal movement and providing gentle elevation. You can find specialized varicocele support underwear that combines scrotal support with cooling properties to address the elevated testicular temperature associated with varicoceles.
Lifestyle modifications include avoiding prolonged standing, maintaining healthy body weight, and using over-the-counter pain relievers when needed. These conservative measures work best for Grade 1 and mild Grade 2 varicoceles without fertility concerns.
Surgical Intervention Criteria
Surgery becomes necessary when you meet specific criteria: palpable varicocele on examination, abnormal semen parameters, documented infertility, and a female partner with normal or treatable fertility factors.
Varicocelectomy improves pregnancy rates and sperm concentration in adult infertile men with any-grade varicoceles. Men who undergo varicocele repair before assisted reproductive technology show significantly higher pregnancy rates (32% vs 11%) and live birth rates (47.6% vs 29.0%) compared to those who proceed with uncorrected varicoceles.
Comparison of Varicocele Grades
What Happens After Treatment
Varicocelectomy outcomes vary by technique, but microsurgical approaches offer the best results with lowest recurrence rates. After surgery, most men experience improvements in sperm concentration within 3-6 months.
Testosterone levels increase following varicocele repair regardless of the initial grade. The number of fast-moving sperm significantly increases after the procedure, though changes in sperm morphology may be less consistent.
Pregnancy rates improve substantially following varicocele correction. Men who undergo varicocelectomy show higher natural conception rates and better outcomes with assisted reproductive techniques compared to those who leave varicoceles untreated.
Frequently Asked Questions
Can Grade 1 varicoceles progress to Grade 2 or 3?
Yes, varicoceles can progress over time, though not all Grade 1 cases worsen. Regular monitoring with your urologist helps track any changes in size or symptoms. If you develop pain, notice testicular size differences, or experience fertility concerns, your doctor may recommend re-evaluation regardless of initial grade.
Does varicocele grade affect which surgical technique is best?
Grade influences surgical planning but doesn’t strictly determine technique. Microsurgical subinguinal or inguinal approaches offer the best outcomes across all grades, with lowest recurrence and complication rates. Your surgeon considers grade along with anatomy, fertility goals, and symptom severity when selecting the optimal repair method.
Should I treat a Grade 2 varicocele if my sperm count is normal?
Current guidelines suggest observation is acceptable for Grade 2 varicoceles when semen parameters are normal and you have no fertility concerns. However, some specialists recommend earlier intervention if you’re planning future children, since varicoceles can cause progressive testicular damage even before abnormal sperm counts appear.