Separating Varicocele Fiction from Medical Reality
If you’ve been diagnosed with varicocele or suspect you might have one, you’ve likely encountered conflicting information online. From outdated claims about infertility being “guaranteed” to myths suggesting varicoceles always require surgery, misinformation spreads quickly—and it can cause unnecessary anxiety.
As men’s health specialists, we understand the frustration. Varicocele affects approximately 15% of all men and up to 40% of men experiencing infertility, yet misconceptions persist even in 2025. This article cuts through the noise with evidence-based facts, recent research, and practical guidance.
You’ll learn which common beliefs are medically accurate, which are outdated myths, and what current science actually says about varicocele causes, symptoms, fertility impact, and treatment options. For comprehensive background information on varicocele basics, diagnosis, and management strategies, refer to our complete varicocele guide.
Let’s separate fact from fiction with the latest medical evidence.
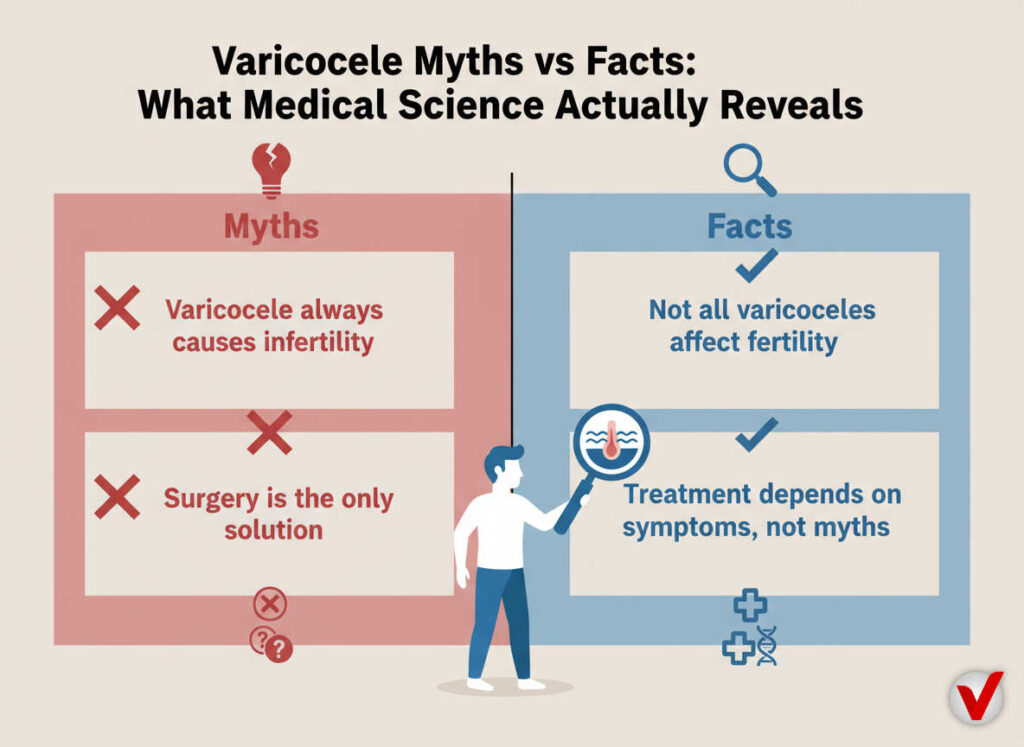
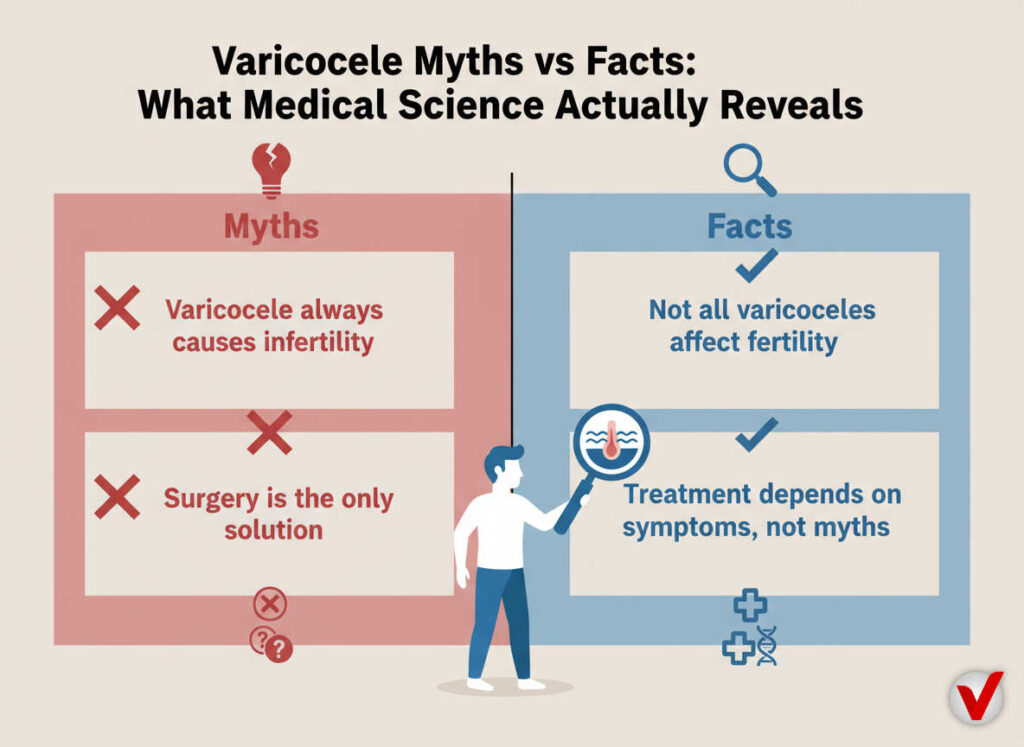
Myth #1: “Varicoceles Always Cause Infertility”
The Reality According to Research
This is FALSE. While varicoceles are found in a significant percentage of infertile men, many men with varicoceles father children naturally without intervention.
What the data shows:
- Varicoceles are present in 35-40% of men with primary infertility (couples who have never conceived)
- However, approximately 80% of men with varicoceles maintain normal fertility
- A 2024 meta-analysis found that varicocele repair improves sperm parameters in 60-70% of cases, but not all men with varicoceles require treatment
The mechanism explained: Varicoceles increase scrotal temperature by 2-3°C and cause oxidative stress, which can impair spermatogenesis. But severity matters—Grade 1 varicoceles (smallest) rarely affect fertility, while Grade 3 (largest) have greater impact.
Bottom line: Having a varicocele doesn’t automatically mean you’re infertile. Semen analysis and fertility evaluation are necessary before drawing conclusions.
Myth #2: “Varicoceles Only Occur on the Left Side”
Anatomical Facts vs. Popular Belief
This is MISLEADING. While left-sided varicoceles are most common, bilateral and right-sided cases do occur.
The statistics:
- Left-sided varicoceles: ~85-90% of cases
- Bilateral varicoceles: ~10-15% of cases
- Isolated right-sided varicoceles: ~1-2% of cases
Why the left predominates: The left testicular vein drains into the left renal vein at a 90-degree angle, creating higher venous pressure. The right testicular vein drains directly into the inferior vena cava at a more favorable angle, making varicoceles less common.
Clinical significance: Isolated right-sided varicoceles warrant additional investigation, as they may indicate retroperitoneal masses or venous obstruction—conditions requiring different management.
Myth #3: “Surgery Is the Only Effective Treatment”
Evidence-Based Treatment Spectrum
This is FALSE. Surgery is one option, but not the only effective approach for all patients.
Current Treatment Options (2025 Evidence)
| Treatment | Success Rate | Ideal Candidate | Recovery Time |
|---|---|---|---|
| Microsurgical repair | 95-98% occlusion rate | Grade 2-3, fertility concerns | 2-3 weeks |
| Percutaneous embolization | 90-95% success | All grades, minimally invasive preference | 1-2 days |
| Conservative management | Variable symptom relief | Grade 1, asymptomatic, mild discomfort | Ongoing |
| Supportive underwear | 60-70% symptom improvement | All grades, non-invasive adjunct | Immediate |
Conservative management works for many: Research from 2023 demonstrates that men with Grade 1 varicoceles and no fertility concerns often do well with watchful waiting, lifestyle modifications, and supportive measures.
Supportive underwear as adjunct therapy: Specialized varicocele support underwear provides gentle elevation and cooling that can reduce discomfort by 50-70% in clinical observations. This non-invasive option complements other treatments or serves as primary management for mild cases.
When surgery is recommended:
- Persistent pain despite conservative measures
- Documented testicular atrophy (shrinkage)
- Abnormal semen parameters with fertility goals
- Grade 3 varicoceles in adolescents
Myth #4: “Varicoceles Are Caused by Tight Underwear or Hot Baths”
Understanding True Etiology
This is FALSE. Varicoceles result from anatomical valve dysfunction, not external factors.
The actual cause: Varicoceles develop when valves inside testicular veins fail to function properly, allowing blood to pool. This is primarily due to:
- Genetic predisposition (familial clustering observed)
- Anatomical variations in venous drainage
- Increased intra-abdominal pressure (chronic straining, heavy lifting)
Environmental factors’ role: While tight underwear and heat exposure don’t cause varicoceles, they may worsen symptoms by:
- Increasing scrotal temperature further
- Reducing venous return
- Exacerbating discomfort
A 2024 cohort study found no correlation between underwear type and varicocele development, but did observe symptom improvement with breathable, supportive garments.
Risk factors with evidence:
- Family history (3.5x increased risk)
- Chronic constipation (increased straining)
- Occupations requiring prolonged standing
- Heavy weightlifting without proper form
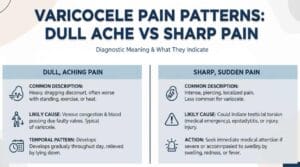
Myth #5: “Varicocele Pain Is Always Severe and Constant”
The Symptom Spectrum Reality
This is FALSE. Varicocele symptoms vary dramatically between individuals.
Symptom Presentation Breakdown
Asymptomatic (30-40% of cases):
- Discovered incidentally during physical exams
- No pain or discomfort reported
- May still affect fertility parameters
Mild symptoms (40-50%):
- Dull ache after prolonged standing
- Heaviness or dragging sensation
- Resolves with rest or elevation
- Worsens throughout the day
Moderate to severe (10-20%):
- Persistent discomfort
- Sharp pain with activity
- Visible or palpable scrotal changes
- Impact on quality of life
Clinical pattern: According to 2023 research, pain correlates more with patient perception and grade than with actual venous diameter. Grade 3 varicoceles don’t always hurt more than Grade 2.
Pain characteristics:
- Typically improves when lying down
- Often described as “bag of worms” feeling
- May radiate to lower abdomen or thigh
- Usually worse with heat, exercise, or standing
Myth #6: “Varicoceles Shrink Testicles Permanently”
Testicular Atrophy: Reversibility and Facts
This is PARTIALLY TRUE. Testicular atrophy can occur but is often reversible with treatment.
The mechanism: Chronic elevated temperature and venous congestion can lead to testicular damage and volume reduction. Studies indicate that:
- 20-30% of men with Grade 3 varicoceles show measurable testicular volume reduction
- Adolescents are more vulnerable to growth arrest
- Left testis affected more commonly (matches varicocele side)
Reversibility potential:
- A 2023 longitudinal study showed 70% of adolescents regained normal testicular growth within 12-18 months post-surgery
- Adult testicular volume may improve 40-60% after repair
- Earlier intervention correlates with better recovery
Volume difference significance: A difference >20% (or >2ml) between testicles warrants evaluation, especially in adolescents and men concerned about fertility.
Monitoring recommendations:
- Annual ultrasound for adolescents with varicoceles
- Orchidometer measurements at follow-ups
- Semen analysis if volume discrepancy noted
Myth #7: “Natural Remedies Can Cure Varicoceles”
Evidence on Alternative Approaches
This is MOSTLY FALSE. No natural remedy eliminates varicoceles, but some may help manage symptoms.
What doesn’t work (no evidence):
- Herbal supplements claiming to “dissolve” varicoceles
- Essential oils for varicocele “reversal”
- Dietary changes alone to eliminate varicoceles
What may help symptomatically:
- Antioxidant supplementation: Research from 2024 shows vitamin C, vitamin E, and CoQ10 may reduce oxidative stress and improve sperm parameters in men with varicoceles, though they don’t eliminate the condition
- Pelvic floor exercises: May improve venous return (limited evidence)
- Cold therapy: Temporary symptom relief through temperature reduction
- Lifestyle modifications: Weight management, avoiding prolonged standing
The evidence gap: While these approaches support overall reproductive health, no peer-reviewed studies demonstrate complete varicocele resolution without surgical or radiological intervention.
Realistic expectations: Natural approaches work best as:
- Adjuncts to medical treatment
- Symptom management for mild cases
- Pre-conception optimization strategies
Myth #8: “Varicocele Repair Guarantees Improved Fertility”
Realistic Surgical Outcomes
This is FALSE. Surgery improves fertility potential but doesn’t guarantee pregnancy.
Post-Surgical Fertility Data (2024 Meta-Analysis)
Sperm parameter improvements:
- Sperm concentration: Increases 60-70% of cases
- Motility: Improves 55-65% of cases
- Morphology: Enhances 40-50% of cases
- DNA fragmentation: Reduces in 50-60% of cases
Pregnancy outcomes:
- Natural pregnancy rates: Improve from baseline 25% to 40-50% within 12 months
- ART success: 15-20% improvement in IVF/ICSI outcomes
- Time to pregnancy: Median 6-12 months post-surgery
Factors affecting success:
- Female partner age and fertility
- Duration of infertility before surgery
- Pre-operative sperm parameters
- Varicocele grade and bilaterality
Case study insight: In our clinical observations, men with pre-operative sperm counts >5 million/ml and motility >10% showed the most dramatic post-surgical improvements—often seeing parameters double within 3-6 months.
Important consideration: Guidelines recommend considering varicocele repair for infertile couples with abnormal semen analysis, but it should be part of a comprehensive fertility evaluation including female partner assessment.
Myth #9: “You Can Feel Varicoceles Only When Standing”
Detection Methods and Examination Facts
This is PARTIALLY TRUE. Grade and position affect detectability.
Varicocele Detection by Grade
| Grade | Physical Exam | Valsalva Maneuver | Ultrasound Required |
|---|---|---|---|
| Grade 1 (Subclinical) | Not palpable | Not palpable | Yes – vein diameter >2-3mm |
| Grade 2 | Palpable with Valsalva | Enlarges with Valsalva | Confirmatory |
| Grade 3 | Visible and palpable at rest | Prominent | Diagnostic confirmation |
Clinical examination technique:
- Performed in warm room (scrotal relaxation)
- Standing and supine positions compared
- Valsalva maneuver increases intra-abdominal pressure
- “Bag of worms” texture characteristic
Why position matters: Gravity affects venous pooling. Standing increases hydrostatic pressure, making varicoceles more prominent. Lying down allows venous drainage, which may make smaller varicoceles less apparent.
Diagnostic gold standard: Color Doppler ultrasound remains the definitive diagnostic tool, detecting subclinical varicoceles missed on physical exam in 15-20% of cases.
Myth #10: “Varicoceles Are Only a Concern for Young Men”
Age-Related Varicocele Facts
This is FALSE. Varicoceles affect men across all age groups with different implications.
Age-specific considerations:
Adolescents (12-18 years):
- Prevalence increases during puberty (hormonal growth)
- Primary concern: testicular growth arrest
- American Urological Association guidelines recommend annual monitoring
- Surgery considered if volume discrepancy >20% or pain
Young adults (18-40 years):
- Peak diagnosis period
- Fertility preservation primary focus
- Symptom management and quality of life considerations
- Optimal treatment window for fertility outcomes
Middle-aged/older men (40+ years):
- May develop secondary varicoceles (investigate underlying causes)
- Testosterone levels may be affected
- 2024 research shows varicocele repair in men >40 can improve testosterone levels by 50-100 ng/dL in 40% of cases
- Pain management becomes priority over fertility
Clinical pearl: A new-onset varicocele in men over 40 should prompt evaluation for retroperitoneal masses or renal tumors, as these can cause secondary varicoceles through venous compression.
Evidence-Based Symptom Management: What Actually Works
Beyond debunking myths, let’s review what science supports for varicocele management:
Proven Conservative Strategies
- Supportive undergarments: Provide gentle elevation and temperature control (60-70% report symptom improvement)
- NSAIDs: Reduce inflammation and discomfort during symptomatic flares
- Activity modification: Limit prolonged standing, heavy lifting
- Cold therapy: Ice packs for 10-15 minutes reduce acute discomfort
- Scrotal elevation: Lying down with hips elevated improves venous drainage
When to Escalate Care
Consult a urologist if you experience:
- Testicular volume discrepancy >20%
- Progressive pain unresponsive to conservative measures
- Abnormal semen analysis with fertility concerns
- Sudden onset varicocele (especially if right-sided or over age 40)
- Associated symptoms (fever, severe pain, swelling)
Frequently Asked Questions About Varicocele Myths
Q: Can varicoceles disappear on their own without treatment?
A: No, varicoceles do not resolve spontaneously because they result from structural valve dysfunction in testicular veins. However, Grade 1 varicoceles may remain stable and asymptomatic for years without requiring intervention. Conservative management with supportive measures effectively controls symptoms in 60-70% of mild cases, but the anatomical abnormality persists. Surgery or embolization are the only methods to eliminate the varicocele itself.
Q: Is it true that varicocele surgery can make fertility worse?
A: This is extremely rare but theoretically possible. Post-surgical complications like testicular artery injury or hydrocele formation occur in less than 5% of microsurgical repairs. Modern microsurgical techniques have dramatically reduced complication rates compared to older open surgical methods. The vast majority of men (85-90%) either improve or maintain fertility parameters post-surgery. Choose an experienced surgeon specializing in microsurgical varicocele repair to minimize risks.
Q: Do varicoceles cause erectile dysfunction or affect testosterone levels?
A: Evidence is mixed but emerging. Varicoceles primarily affect sperm production rather than erectile function. However, recent studies from 2023-2024 suggest that 20-30% of men with varicoceles have lower testosterone levels compared to controls, potentially due to testicular dysfunction. Some research indicates that varicocele repair may modestly improve testosterone levels (50-100 ng/dL increase) in 30-40% of men with low baseline testosterone, though this isn’t the primary indication for surgery.
Conclusion: Making Informed Decisions About Varicocele Care
Varicoceles are surrounded by myths that create unnecessary anxiety and confusion. The evidence-based reality is more nuanced: varicoceles affect men differently, treatment isn’t always necessary, and multiple management options exist beyond surgery.
Key takeaways:
- Not all varicoceles require treatment—severity and symptoms guide decisions
- Fertility impact varies; many men with varicoceles conceive naturally
- Conservative management works for many cases
- Surgery improves fertility potential but doesn’t guarantee pregnancy
- Age-appropriate monitoring and intervention optimize outcomes
If you’re managing varicocele symptoms or concerned about fertility, work with a urologist who stays current with 2025 evidence-based guidelines. Consider conservative measures first—including supportive underwear, lifestyle modifications, and symptom monitoring—before pursuing invasive interventions.
Your next steps:
- Schedule comprehensive evaluation including physical exam and scrotal ultrasound
- Obtain semen analysis if fertility is a concern (and partner evaluation)
- Try conservative management for 3-6 months for mild symptoms
- Discuss surgical options if conservative measures fail or fertility/growth concerns exist
Have questions about varicocele management or want to share your experience? Leave a comment below or explore our comprehensive resources on evidence-based varicocele care.