Living with varicocele—a condition affecting up to 15% of men—goes far beyond physical discomfort. While medical discussions typically focus on testicular pain, fertility concerns, and surgical interventions, the profound psychological toll often remains unaddressed. If you’re experiencing anxiety, depression, body image concerns, or relationship stress alongside your varicocele diagnosis, you’re not alone, and your mental health struggles are valid.
This comprehensive guide explores the bidirectional relationship between varicocele and mental health, backed by current research and clinical insights. You’ll discover why this vascular condition affects emotional wellbeing, learn evidence-based coping strategies, understand when treatment becomes necessary, and find actionable steps to reclaim both your physical and psychological health. Whether you’ve just been diagnosed or have lived with varicocele for years, understanding this mind-body connection is essential for holistic healing.
Understanding Varicocele: Physical Foundation of Psychological Impact
What Is Varicocele and Who Does It Affect?
Varicocele represents an enlargement of veins within the scrotum, similar to varicose veins that occur in legs. The condition affects approximately 15% of the general male population, with prevalence increasing to 35-40% among men evaluated for primary infertility and up to 80% in those with secondary infertility.
The condition develops when valves inside the spermatic cord veins malfunction, causing blood to pool rather than circulate efficiently. This pooling creates visible, palpable enlargement—often described as feeling like “a bag of worms”—typically on the left side due to anatomical differences in venous drainage.
Key demographic patterns include:
- Age of onset: Most commonly develops during puberty (ages 15-25) when rapid growth stresses the venous system
- Left-sided predominance: 85-90% occur on the left side, 10% bilaterally, and less than 2% exclusively right-sided
- Fertility impact: Present in 35-44% of men with primary infertility according to research published in the Asian Journal of Andrology
- Grade classification: Ranges from Grade I (palpable only during Valsalva maneuver) to Grade III (visible through scrotal skin)
The Physical Symptoms That Trigger Psychological Distress
Understanding the physical manifestations helps contextualize why varicocele so significantly impacts mental health. Common symptoms include:
Pain and discomfort (experienced by 2-10% of affected men):
- Dull, aching sensation that worsens with prolonged standing or physical exertion
- Heavy or dragging feeling in the scrotum, particularly at day’s end
- Sharp or shooting pain during or after physical activity
- Discomfort that improves when lying down
Visible changes:
- Noticeable asymmetry between testicles
- Visible venous enlargement, especially when standing
- Testicular atrophy (shrinkage) on the affected side
- Changes in scrotal skin appearance or texture
Fertility concerns:
- Abnormal semen parameters in 70-80% of men with varicocele
- Reduced sperm count, motility, and morphology
- Elevated levels of oxidative stress affecting sperm DNA integrity
- Progressive decline in testicular function if left untreated
These physical realities create a foundation for psychological distress that extends far beyond the medical chart.
The Psychological Burden: How Varicocele Affects Mental Health
Anxiety Disorders and Varicocele: A Clinical Connection
The relationship between varicocele and anxiety manifests across multiple domains, with research increasingly documenting this association. A 2023 study in the International Journal of Impotence Research found that men with varicocele demonstrated significantly higher anxiety scores compared to controls, with anxiety levels correlating with varicocele grade severity.
Primary anxiety manifestations include:
Health anxiety (hypochondriasis):
- Excessive worry about testicular cancer risk, despite varicocele being benign
- Frequent self-examination leading to heightened body vigilance
- Catastrophic thinking about worst-case scenarios
- Compulsive online research creating information overload and confusion
Fertility-related anxiety:
- Obsessive concern about ability to father children
- Anticipatory grief over potential infertility
- Relationship strain due to fertility uncertainty
- Anxiety about “letting down” partners or family expectations
Performance anxiety:
- Fear of pain during sexual activity
- Worry about visible scrotal changes being noticed by partners
- Concern about reduced testosterone affecting sexual function
- Anticipatory anxiety about physical activities triggering pain
Treatment decision anxiety:
- Uncertainty about whether surgery is necessary
- Fear of surgical complications or unsuccessful outcomes
- Anxiety about recovery time and activity restrictions
- Financial stress regarding treatment costs
Clinical experience reveals that anxiety often intensifies during waiting periods—between diagnosis and consultation, or after treatment while awaiting fertility assessment—when uncertainty peaks and control feels minimal.
Depression and Mood Disorders: The Emotional Toll
Depression represents another significant psychological consequence of living with varicocele. Research published in Urology demonstrated that men with varicocele-related infertility showed elevated depression scores, with improvement following surgical correction.
Depressive symptoms commonly observed include:
Emotional symptoms:
- Persistent sadness or emptiness related to diagnosis
- Loss of interest in previously enjoyable activities
- Feelings of hopelessness about fertility or symptom resolution
- Irritability and frustration with chronic discomfort
- Emotional numbness or detachment
Cognitive symptoms:
- Difficulty concentrating on work or daily tasks
- Rumination about the condition and its implications
- Negative self-talk and self-blame
- Decision-making paralysis regarding treatment options
- Memory difficulties potentially linked to chronic stress
Physical symptoms:
- Fatigue beyond what physical symptoms explain
- Sleep disturbances (insomnia or hypersomnia)
- Changes in appetite or weight
- Decreased energy and motivation
- Psychosomatic pain amplification
Social withdrawal:
- Avoiding intimate relationships due to body shame
- Withdrawing from sports or physical activities
- Isolating from friends to avoid discussing the condition
- Reluctance to seek medical help due to embarrassment
The relationship between varicocele and depression appears bidirectional—chronic physical symptoms contribute to mood disorders, while depression can amplify pain perception and reduce treatment adherence.
Body Image Disturbance and Masculine Identity Crisis
Perhaps no psychological impact of varicocele receives less clinical attention than body image disturbance, despite its profound effects on self-concept and quality of life.
Genital body image concerns:
Men with varicocele frequently report distress about:
- Visible asymmetry between testicles
- Enlarged, “abnormal-looking” veins in the scrotum
- Testicular atrophy creating size discrepancy
- Fear of partner reactions to appearance
- Avoidance of situations requiring nudity (locker rooms, intimacy, medical exams)
Research in Body Image journal confirms that genital appearance concerns significantly impact male psychological wellbeing, yet men rarely receive support for these issues within medical settings.
Masculinity and identity challenges:
Varicocele can trigger deeper questions about masculine identity:
- Fertility as manhood: Cultural equations of virility with reproductive capacity create existential distress when fertility is threatened
- Physical capability: Chronic pain or exercise limitations challenge self-concepts built on physical strength or athletic performance
- Sexual confidence: Concerns about reduced testosterone, erectile function, or genital appearance undermine sexual self-assurance
- Silence and stoicism: Traditional masculine norms discourage vulnerability, creating isolation and preventing help-seeking
One patient in our clinical practice described feeling “defective as a man” after diagnosis, despite the condition’s high prevalence. This reflects broader cultural narratives that equate male worth with reproductive and sexual function, creating psychological vulnerability when these capacities feel threatened.
Relationship Stress and Intimacy Challenges
Varicocele ripples outward, affecting romantic relationships and intimate connections in multiple ways:
Communication barriers:
- Difficulty discussing the condition with partners due to embarrassment
- Avoiding conversations about fertility implications
- Withholding concerns to protect partners from worry
- Misunderstandings when physical symptoms affect availability or mood
Sexual relationship impacts:
- Reduced sexual frequency due to pain or anxiety
- Performance pressure and erectile difficulties
- Self-consciousness during intimate moments
- Partner confusion or concern when sexual patterns change
Fertility journey stress:
- Guilt about being the “cause” of fertility challenges
- Tension during fertility testing and treatment
- Emotional distance if partners cope differently
- Relationship questioning: “Should my partner be with someone without this condition?”
Partner psychological burden:
- Secondary anxiety about fertility outcomes
- Feeling helpless to relieve partner’s distress
- Navigating medical decisions together
- Balancing support with maintaining own emotional health
Studies in Fertility and Sterility document that male factor infertility, including varicocele, creates psychological distress for both partners, with relationship satisfaction declining when communication remains closed or blame-oriented.
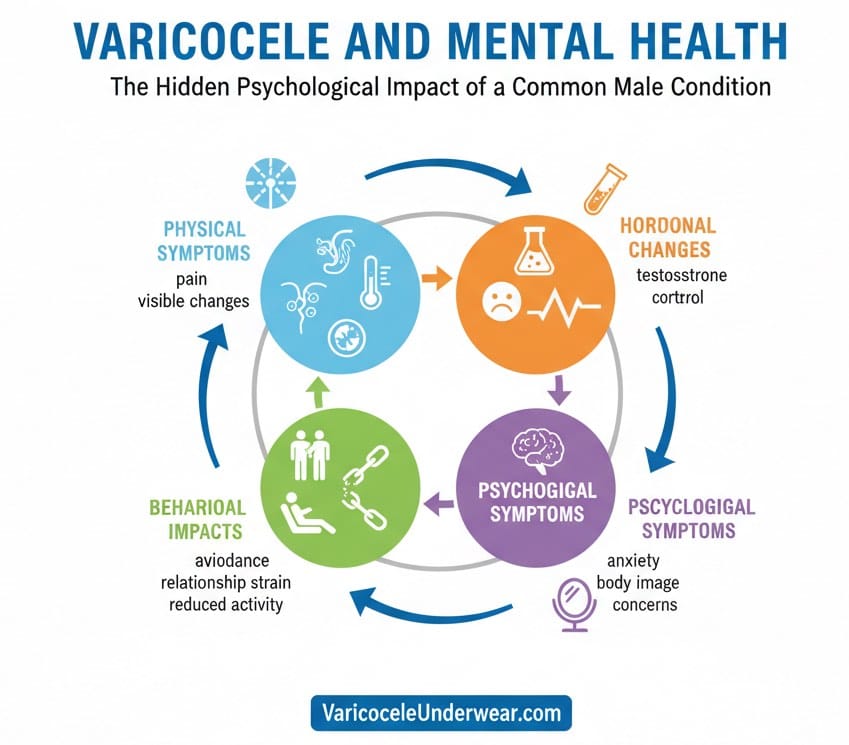
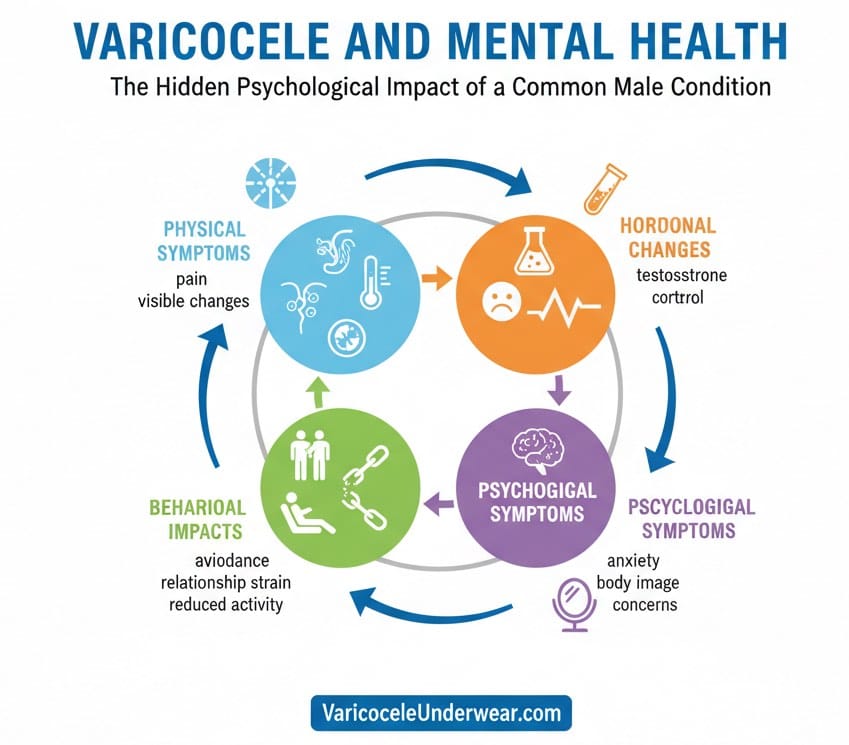
The Psychophysiological Mechanisms: Why Varicocele Affects Mental Health
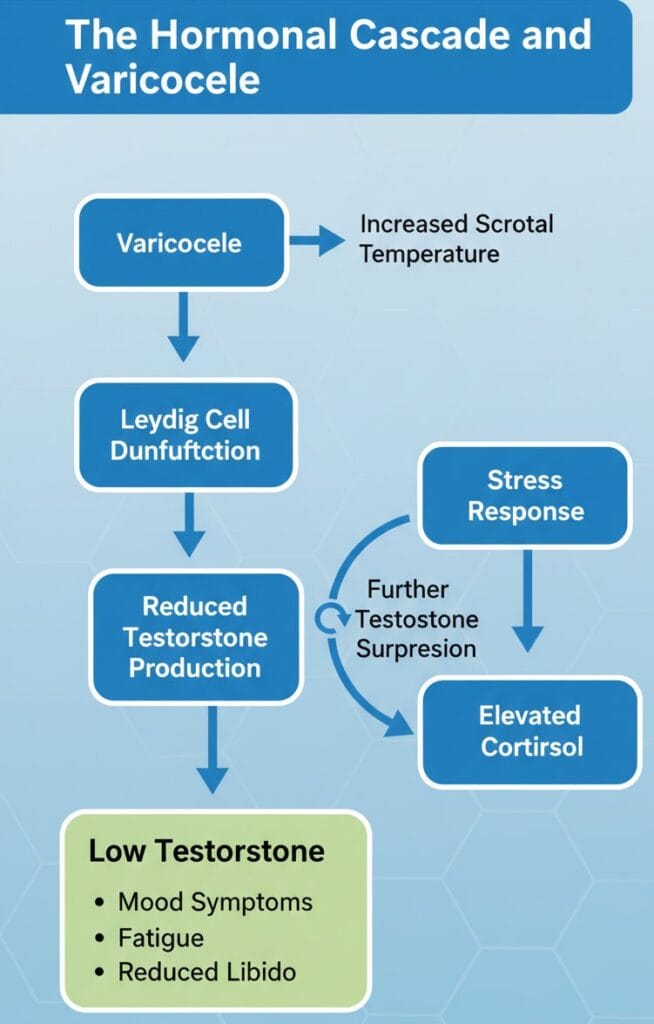
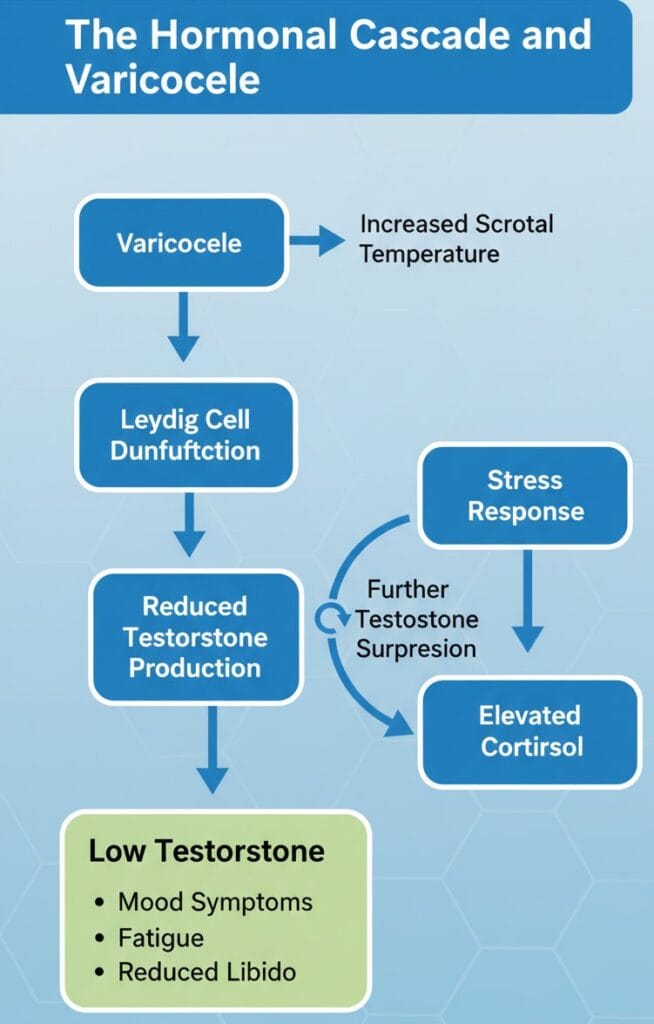
Hormonal Pathways: Testosterone, Stress, and Mood
The connection between varicocele and mental health operates partially through hormonal mechanisms, particularly involving testosterone and the hypothalamic-pituitary-gonadal (HPG) axis.
Testosterone and psychological wellbeing:
Research indicates that varicocele can reduce testosterone levels through several mechanisms:
- Increased scrotal temperature impairing Leydig cell function
- Oxidative stress damaging testosterone-producing cells
- Venous hypertension affecting testicular microenvironment
- Progressive testicular atrophy reducing hormone production capacity
Low testosterone associates with:
- Increased risk of depression and anxiety disorders
- Reduced energy, motivation, and cognitive function
- Decreased libido and sexual confidence
- Changes in body composition affecting self-image
- Potential impacts on stress resilience
Stress hormone dysregulation:
Chronic pain and illness-related stress activate the hypothalamic-pituitary-adrenal (HPA) axis, elevating cortisol production. Sustained cortisol elevation contributes to:
- Mood disorders including anxiety and depression
- Sleep disturbances and fatigue
- Cognitive difficulties including memory and concentration
- Further suppression of testosterone production
- Immune system dysregulation
This creates a vicious cycle: varicocele → hormonal changes → psychological symptoms → stress → worsened hormonal function.
Chronic Pain and Central Sensitization
For the subset of men experiencing chronic varicocele pain, neurobiological changes amplify both physical and psychological suffering.
Pain processing alterations:
Chronic pain conditions trigger central sensitization—changes in nervous system processing that:
- Lower pain thresholds (normal sensations feel painful)
- Expand pain areas (spreading beyond the original site)
- Prolong pain after stimuli cease
- Create hypervigilance to bodily sensations
These changes are documented across chronic pain conditions and explain why some men with relatively mild physical varicocele findings experience disproportionate pain and distress.
Pain-mood bidirectional relationship:
Research in Pain Medicine confirms that chronic pain and depression share neurobiological pathways:
- Both involve altered neurotransmitter function (serotonin, norepinephrine, dopamine)
- Shared brain regions process physical pain and emotional distress (anterior cingulate cortex, insula)
- Depression lowers pain tolerance while pain increases depression risk
- Sleep disturbance—common in both—amplifies both conditions
Inflammation and the Gut-Brain Axis
Emerging research suggests inflammation may link varicocele with psychological symptoms through the gut-brain axis.
Oxidative stress and inflammation:
Varicocele creates an environment of:
- Elevated reactive oxygen species (ROS) in testicular tissue
- Systemic inflammatory markers including C-reactive protein
- Potential gut microbiome alterations through stress-induced changes
Inflammation-depression connection:
Extensive research documented in Brain, Behavior, and Immunity demonstrates that:
- Inflammatory cytokines can trigger depressive symptoms
- Inflammation affects neurotransmitter metabolism
- Chronic inflammation correlates with treatment-resistant depression
- Anti-inflammatory interventions can improve mood in some patients
While research specifically linking varicocele inflammation to mood disorders remains limited, the mechanisms suggest plausible connections warranting further investigation.
Clinical Evidence: Research on Varicocele and Psychological Outcomes
Studies Documenting Mental Health Impact
The past decade has seen increasing research attention to psychological dimensions of varicocele:
Quality of life assessments:
A 2019 systematic review in Translational Andrology and Urology analyzed quality of life in men with varicocele, finding:
- Significantly reduced scores on physical functioning, bodily pain, and vitality domains
- Emotional wellbeing scores correlated inversely with symptom severity
- Sexual function concerns contributed substantially to reduced quality of life
- Improvement in psychological measures following successful treatment
Anxiety and depression prevalence:
Research using validated psychological instruments reveals:
- Hospital Anxiety and Depression Scale (HADS) scores significantly elevated in varicocele patients versus controls
- Beck Depression Inventory scores higher in men with varicocele-related infertility
- State-Trait Anxiety Inventory revealing elevated trait anxiety in affected men
- Correlation between varicocele grade and psychological symptom severity
Fertility distress studies:
Research in Human Reproduction documents that:
- Male factor infertility, including varicocele, creates comparable distress to female factors
- Men report feeling guilt, inadequacy, and reduced masculinity
- Psychological support improves coping and relationship satisfaction
- Untreated psychological symptoms predict poorer fertility treatment adherence
Post-Treatment Psychological Outcomes
An encouraging body of evidence demonstrates psychological improvement following varicocele treatment:
Surgical intervention studies:
Research published in Urology Annals found:
- Significant reduction in anxiety and depression scores 3-6 months post-varicocelectomy
- Improvement in quality of life measures across multiple domains
- Enhanced sexual satisfaction and confidence
- Benefits evident even in men whose fertility parameters didn’t significantly improve
Pain resolution and mental health:
Studies examining men treated primarily for pain reveal:
- 70-90% report pain improvement following microsurgical varicocelectomy
- Psychological symptom improvement correlated with pain relief
- Return to physical activities associated with improved mood and self-efficacy
- Quality of life gains sustained at 1-2 year follow-up
Fertility success and psychological relief:
Data from the Journal of Urology indicates:
- Pregnancy achievement following varicocele repair associates with substantial psychological relief
- Even improved semen parameters without immediate pregnancy reduce anxiety
- Couples report improved relationship satisfaction post-treatment
- Psychological benefits appear independent of treatment modality (surgery vs. embolization)
Gaps in Current Research
Despite growing evidence, significant research gaps remain:
- Limited prospective studies: Most research is retrospective or cross-sectional, limiting causal inferences
- Lack of intervention trials: Few studies test psychological interventions alongside medical treatment
- Cultural diversity: Most research involves Western populations; experience in diverse cultural contexts remains understudied
- Long-term outcomes: Limited data on psychological wellbeing 5-10 years post-diagnosis or treatment
- Mechanism studies: Insufficient research on specific biological pathways linking varicocele to mental health
Coping Strategies: Managing the Psychological Impact
Professional Mental Health Support


Seeking psychological help for varicocele-related distress is not weakness—it’s evidence-based self-care.
When to seek professional help:
Consider consulting a mental health professional if you experience:
- Persistent sadness, hopelessness, or anxiety lasting more than two weeks
- Symptoms interfering with work, relationships, or daily functioning
- Sleep disturbances or appetite changes
- Social withdrawal or loss of interest in previously enjoyed activities
- Thoughts of self-harm or feeling life isn’t worth living
- Relationship conflict related to the condition
- Difficulty making treatment decisions due to overwhelming anxiety
Types of mental health professionals:
- Psychologists: Provide evidence-based psychotherapy; PhD or PsyD trained
- Psychiatrists: Medical doctors who can prescribe medication and provide therapy
- Licensed clinical social workers (LCSW): Offer counseling and connect clients with resources
- Licensed professional counselors (LPC): Provide therapy across various modalities
- Sex therapists: Specialize in sexual and relationship concerns related to medical conditions
Evidence-based therapeutic approaches:
Cognitive-Behavioral Therapy (CBT):
- Identifies and challenges unhelpful thought patterns (“I’m defective,” “This will ruin my life”)
- Develops coping skills for managing anxiety and pain
- Addresses avoidance behaviors maintaining distress
- Extensive evidence supports CBT for health-related anxiety and depression
Acceptance and Commitment Therapy (ACT):
- Helps individuals accept what cannot be controlled while taking valued action
- Reduces struggle against distressing thoughts and feelings
- Clarifies personal values and aligns behavior accordingly
- Particularly effective for chronic pain and health conditions
Couples therapy:
- Improves communication about the condition and its impacts
- Addresses sexual concerns and intimacy challenges
- Reduces blame and increases mutual support
- Navigates fertility decisions collaboratively
Mindfulness-based interventions:
- Reduces rumination and worry through present-moment awareness
- Improves pain tolerance and reduces suffering
- Decreases physiological stress responses
- Evidence demonstrates effectiveness for anxiety, depression, and chronic pain
Self-Care and Lifestyle Interventions
Evidence-based self-care strategies can substantially improve psychological wellbeing:
Physical activity and exercise:
- Aim for 150 minutes of moderate aerobic activity weekly
- Include resistance training 2-3 times weekly
- Choose activities that don’t exacerbate varicocele pain (swimming, cycling may be better than running)
- Exercise releases endorphins, reduces inflammation, and improves sleep
- Group activities provide social connection and accountability
Sleep hygiene optimization:
Quality sleep is essential for mental health:
- Maintain consistent sleep-wake times, even on weekends
- Create a dark, cool, quiet sleep environment
- Limit screen time 1-2 hours before bed
- Avoid caffeine after 2 PM and alcohol close to bedtime
- Address pain that interrupts sleep through positioning, supportive underwear, or medical consultation
Nutrition and anti-inflammatory diet:
Dietary choices influence both physical symptoms and mental health:
- Emphasize anti-inflammatory foods: fatty fish, colorful vegetables, berries, nuts, olive oil
- Limit processed foods, excess sugar, and trans fats
- Ensure adequate protein for tissue repair and neurotransmitter synthesis
- Stay hydrated—dehydration worsens both pain and mood
- Consider Mediterranean-style eating pattern, linked to reduced depression risk
Stress management techniques:
- Deep breathing: Activates parasympathetic nervous system, reducing anxiety rapidly
- Progressive muscle relaxation: Releases physical tension contributing to pain
- Journaling: Processes emotions and identifies thought patterns
- Time in nature: Documented to reduce cortisol and improve mood
- Creative outlets: Music, art, writing provide emotional expression and distraction
Supportive underwear and symptom management:
Physical comfort directly impacts psychological wellbeing. Specialized supportive underwear designed for varicocele can provide:
- Gentle elevation reducing venous pooling and discomfort
- Temperature regulation addressing heat-related symptoms
- Improved confidence during physical and social activities
- Non-invasive symptom relief while considering treatment options
This simple intervention often reduces the daily physical reminders that trigger psychological distress.
Communication Strategies: Talking About Varicocele
Breaking silence reduces psychological burden significantly.
Communicating with partners:
- Choose the right timing: Not during conflict or immediately before intimacy
- Be honest about impacts: Share how the condition affects you physically and emotionally
- Educate together: Share reliable resources so partners understand the condition
- Discuss fertility implications: Address concerns openly rather than avoiding difficult topics
- Request specific support: Partners can’t read minds; say what would be helpful
- Maintain intimacy: Find ways to connect sexually and emotionally that feel comfortable
Discussing with healthcare providers:
Many men minimize psychological symptoms during medical appointments. To advocate effectively:
- Prepare written notes: Symptoms often forgotten under appointment pressure
- Be specific: “I’ve had daily anxiety for three months” is more actionable than “I’m stressed”
- Ask directly: “Could this be affecting my mood?” or “Should I see a mental health professional?”
- Bring partners: They often notice symptoms and impacts you’ve normalized
- Request referrals: Ask about mental health resources, support groups, or specialized counselors
Selective disclosure to friends/family:
You’re not obligated to share widely, but trusted support is valuable:
- Choose 1-2 people who have demonstrated trustworthiness and empathy
- Share what feels comfortable; you control the level of detail
- Be clear about what you need: listening, advice, or simply acknowledgment
- Set boundaries around privacy—ask that information not be shared further
Treatment Decisions: Navigating Physical and Psychological Factors
When to Consider Varicocele Treatment
Treatment decisions involve both medical and psychological considerations.
Medical indications for treatment:
According to American Urological Association guidelines:
- Documented abnormal semen parameters in men attempting conception
- Testicular atrophy or size discrepancy
- Progressive decline in testicular function
- Chronic pain significantly impacting quality of life
- Clinical varicocele in adolescents with arrested testicular growth
Psychological indications for treatment:
Even without strict medical necessity, treatment may be appropriate when:
- Anxiety or depression substantially impairs functioning
- Body image concerns prevent intimate relationships
- Constant worry about the condition dominates daily life
- Conservative management has failed to relieve psychological distress
- The condition creates relationship strain
Clinical experience suggests that combining medical and psychological criteria provides the most comprehensive decision framework.
Treatment Options Overview
Surgical interventions:
- Microsurgical varicocelectomy: Gold standard with 95% success rates and lowest recurrence
- Laparoscopic varicocelectomy: Minimally invasive with good outcomes
- Open surgical approaches: Various techniques with varying success rates
Percutaneous embolization:
- Non-surgical option performed by interventional radiologists
- Similar effectiveness to surgery with faster recovery
- May have slightly higher recurrence rates
Conservative management:
- Supportive underwear and lifestyle modifications
- Pain management with NSAIDs
- Temperature regulation strategies
- Regular monitoring without immediate intervention
Psychological treatment:
- May be primary intervention or adjunct to physical treatment
- Addresses symptoms regardless of treatment choice
- Improves coping and decision-making capacity
Integrating Physical and Psychological Treatment
The most effective approach often combines interventions:
Pre-treatment psychological preparation:
- Address anxiety about procedure and outcomes
- Establish realistic expectations
- Develop coping strategies for recovery period
- Strengthen support systems
Concurrent psychological support:
- Continue therapy through treatment and recovery
- Process emotions arising during medical procedures
- Manage pain and discomfort during healing
- Address any disappointment if results don’t meet expectations
Post-treatment psychological follow-up:
- Monitor for persistent or new psychological symptoms
- Celebrate improvements while managing ongoing concerns
- Address any residual body image or fertility concerns
- Support relationship healing and reconnection
Research in the Journal of Sexual Medicine confirms that integrating psychological care with medical treatment optimizes both physical and mental health outcomes.
Special Populations and Considerations
Adolescents and Young Men
Varicocele diagnosis during adolescence or early adulthood poses unique psychological challenges.
Developmental impacts:
- Identity formation disrupted during critical period
- Peer comparison and fitting in become fraught
- Emerging sexuality complicated by body image concerns
- Future fertility concerns may feel abstract yet anxiety-provoking
Parental involvement:
- Parents often accompany young patients, requiring navigation of privacy and autonomy
- Communication between parents, adolescents, and providers needs coordination
- Family anxiety can amplify adolescent distress
Treatment considerations:
- Earlier intervention may prevent testicular damage
- Psychological impact of untreated condition versus surgical experience
- Long-term fertility preservation as primary goal
Support strategies:
- Age-appropriate education materials
- Peer support groups or online communities
- School accommodations if pain interferes with activities
- Mental health screening and early intervention
Men in Fertility Treatment
Men undergoing fertility evaluation and treatment face compounded psychological stress.
Unique stressors:
- Identity threat when male factor contributes to infertility
- Pressure of semen analysis and repeated testing
- Treatment timing creating performance anxiety
- Financial burden of fertility procedures
- Relationship strain during emotionally charged journey
Evidence-based support:
- Couples counseling improves communication and reduces blame
- Male-specific support groups normalize experience
- Stress reduction techniques improve semen parameters in some men
- Realistic expectation-setting about varicocele repair outcomes (improvement likely, pregnancy not guaranteed)
Cultural and Diversity Considerations
Psychological experience of varicocele varies across cultural contexts.
Cultural factors influencing experience:
- Fertility’s central role in masculine identity varies across cultures
- Medical help-seeking norms differ
- Mental health stigma varies in severity
- Communication norms about sexual/reproductive health differ
- Religious beliefs may influence treatment decisions
Healthcare provider responsibilities:
- Cultural humility and avoiding assumptions
- Provision of interpretation services when needed
- Understanding how cultural background shapes distress and coping
- Respectful inquiry about beliefs influencing treatment preferences
Building a Comprehensive Care Plan
The Multidisciplinary Approach
Optimal care for varicocele—particularly when psychological impact is significant—involves coordination across specialties.
Core team members:
- Urologist or andrologist: Primary medical management, treatment decisions
- Mental health professional: Addresses psychological symptoms, provides therapy
- Primary care physician: Coordinates care, manages overall health
- Fertility specialist (if relevant): Guides conception attempts, manages assisted reproduction
- Pain specialist (if relevant): For complex or refractory pain management
Communication between providers:
- Integrated care requires information sharing (with patient consent)
- Shared treatment goals across disciplines
- Awareness of how each intervention affects others
- Coordinated timing of interventions
Creating Your Personal Action Plan
A concrete action plan empowers proactive management:
Step 1: Comprehensive assessment
- Complete medical evaluation with urologist
- Mental health screening (consider validated questionnaires like PHQ-9 for depression, GAD-7 for anxiety)
- Relationship assessment if partnered
- Quality of life evaluation
Step 2: Prioritize concerns
- Rank your most distressing symptoms (physical and psychological)
- Identify which issues most impair functioning
- Determine what outcomes matter most to you
Step 3: Set specific goals
- “Reduce anxiety enough to sleep through the night”
- “Feel comfortable being intimate with my partner”
- “Make a treatment decision within two months”
- “Improve relationship communication about fertility”
Step 4: Implement interventions
- Schedule appointments with identified providers
- Begin lifestyle modifications (exercise, sleep hygiene, supportive underwear)
- Start therapy or counseling
- Join support groups or communities
Step 5: Monitor and adjust
- Track symptoms using apps, journals, or scales
- Reassess every 4-6 weeks
- Adjust strategies based on what’s working
- Don’t hesitate to try different approaches
Resources and Support
Reputable online information:
- American Urological Association patient education
- Mayo Clinic varicocele information
- National Institute of Health (NIH) resources
- American Society for Reproductive Medicine
Mental health resources:
- Psychology Today therapist directory (find specialists in health anxiety, chronic pain, fertility stress)
- Better Help or Talkspace for online therapy options
- National Alliance on Mental Illness (NAMI) for support groups and education
- Mental Health America screening tools
Support communities:
- Reddit communities (r/varicocele) for peer support
- Male fertility support groups (often found through fertility clinics)
- Chronic pain support groups
- Online forums moderated by medical professionals
Frequently Asked Questions
Can varicocele directly cause depression, or is the psychological impact just from dealing with a medical condition?
The relationship is likely multifaceted. While some psychological distress stems from coping with symptoms and diagnostic uncertainty, emerging evidence suggests biological mechanisms may directly contribute. Varicocele can reduce testosterone levels, and low testosterone associates with increased depression risk. Additionally, chronic pain conditions alter brain chemistry and function in ways that increase vulnerability to mood disorders. Inflammation and oxidative stress associated with varicocele may also influence mental health through the gut-brain axis and systemic inflammatory pathways. Most likely, both direct biological effects and the psychological challenge of managing symptoms contribute together to mental health impact.
Will treating my varicocele automatically improve my mental health, or do I need separate psychological treatment?
Research shows that successful varicocele treatment—whether surgical or embolization—typically improves psychological symptoms like anxiety and depression, particularly when pain reduction or fertility improvement occurs. However, improvement isn’t universal or immediate. Psychological symptoms may persist due to ingrained thought patterns, relationship damage requiring repair, or independent mental health conditions. The most effective approach usually combines medical treatment for varicocele with concurrent or subsequent psychological support. Think of it as treating both the physical foundation and the psychological impacts that developed, rather than expecting one intervention to automatically resolve everything.
How can I tell if my anxiety about varicocele is “normal worry” versus something requiring professional help?
Consider these factors: Frequency—do you think about the varicocele multiple times daily, interfering with focus on work or relationships? Duration—has the distress persisted for weeks or months without improvement? Intensity—does the anxiety cause physical symptoms like rapid heartbeat, insomnia, or digestive issues? Avoidance—are you avoiding activities, relationships, or decisions because of varicocele-related fears? Functioning—is your ability to work, maintain relationships, or care for yourself impaired? If you answered yes to multiple questions, professional support would likely be beneficial. Even if your worry seems “reasonable,” professional help can provide coping strategies and reduce suffering.
Conclusion: Toward Holistic Healing
Living with varicocele challenges both body and mind, but you don’t have to face these challenges alone or in silence. The psychological impacts—anxiety, depression, body image concerns, relationship stress—are real, valid, and deserving of attention alongside physical symptoms.
Current evidence makes clear that varicocele affects mental health through multiple pathways: hormonal changes, chronic pain, fertility concerns, and the psychological burden of managing an intimate health condition. Equally important, research confirms that effective intervention—whether medical treatment, psychological support, lifestyle modification, or typically a combination—can substantially improve both physical symptoms and psychological wellbeing.
Your path forward begins with acknowledgment: recognizing that the emotional toll you’re experiencing is neither weakness nor overreaction, but a legitimate response to a real medical condition. From this foundation, you can build a comprehensive care plan that addresses both the physical varicocele and its psychological reverberations.
Whether you choose immediate treatment or careful monitoring, consider supportive interventions like specialized underwear, prioritize mental health alongside physical health, and open communication channels with partners and healthcare providers, you’re taking active steps toward reclaiming wellbeing. The journey may not always be linear, but with integrated care, self-compassion, and appropriate support, improvement is not just possible—it’s probable.
You deserve care that addresses the whole you, not just a set of symptoms. Reach out, speak up, and remember: healing encompasses both body and mind.