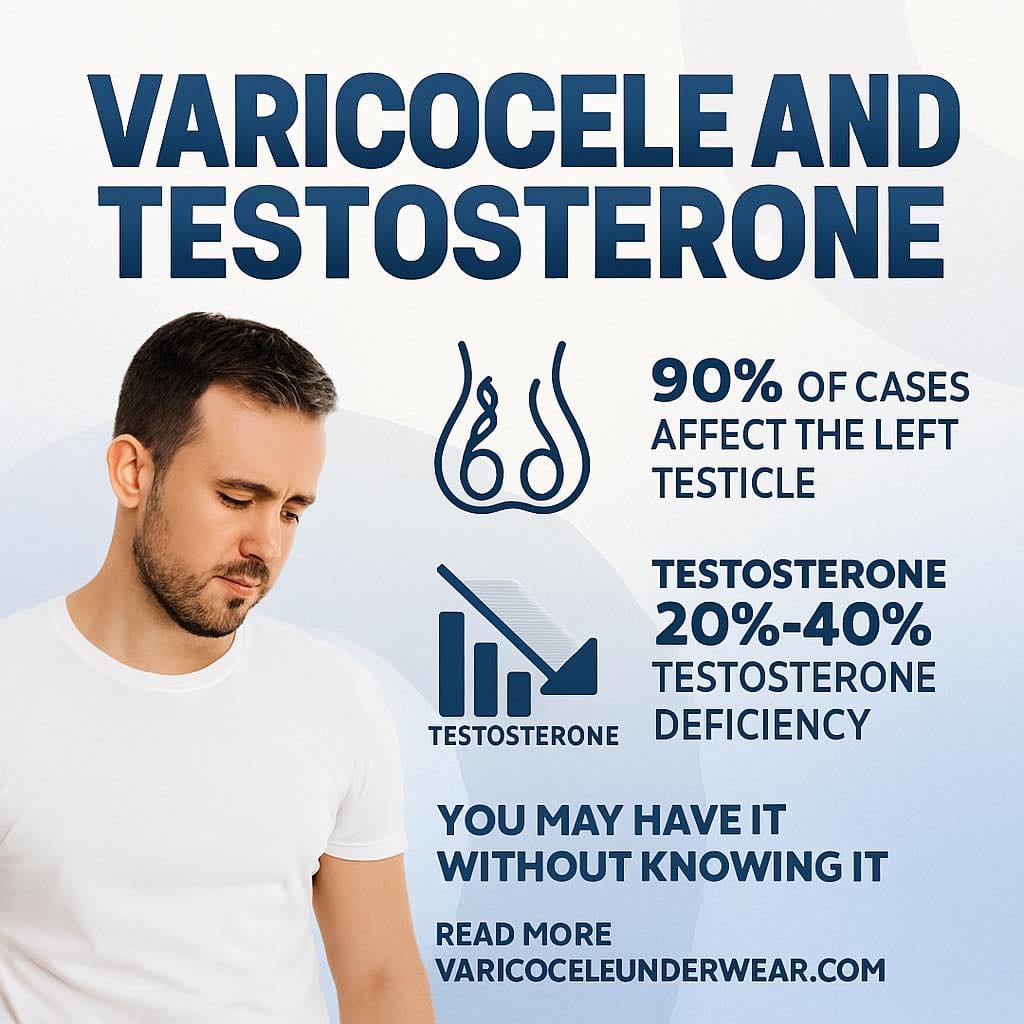
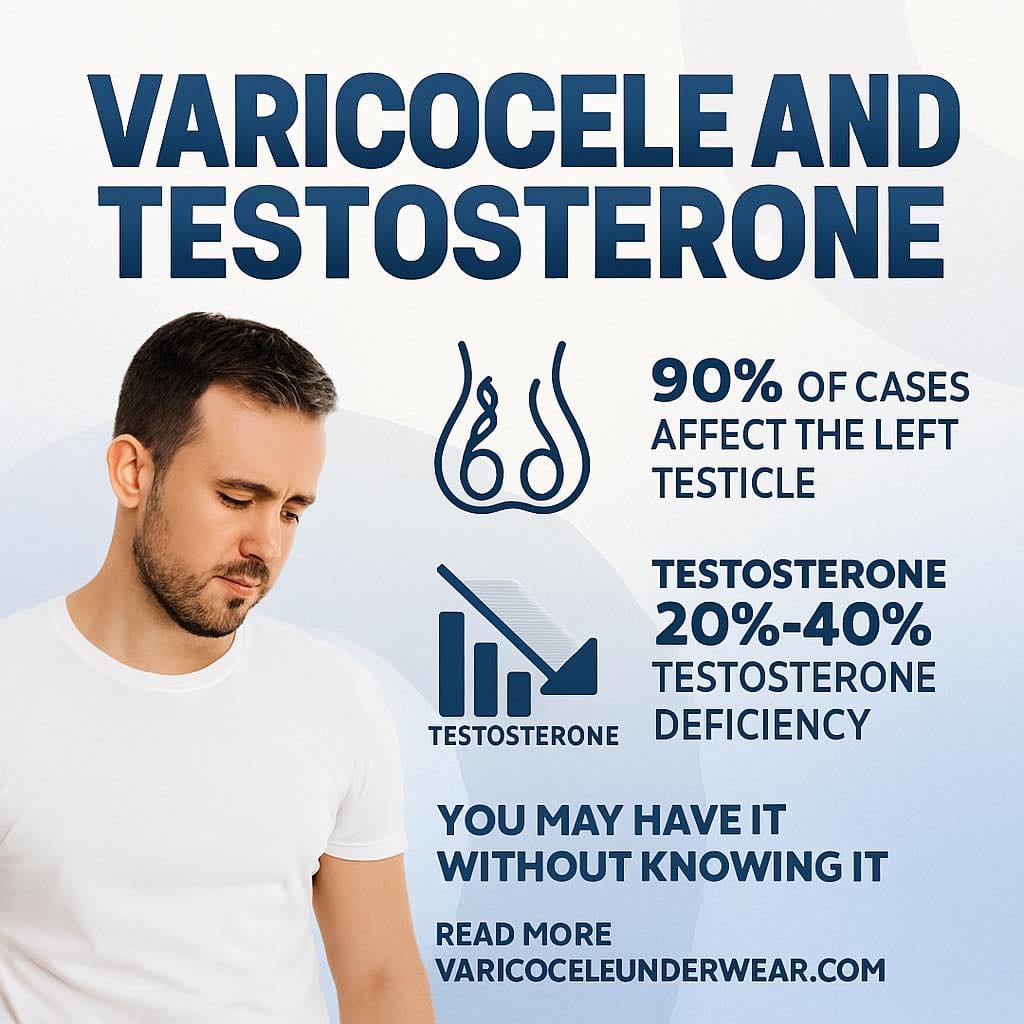
If you’ve been diagnosed with a varicocele, you may have noticed symptoms beyond the visible swelling or discomfort—like decreased energy, reduced muscle mass, or changes in libido. These could signal testosterone deficiency, a common yet often overlooked consequence of varicoceles. Understanding the connection between varicoceles and testosterone levels is crucial for men’s health, especially since approximately 15% of men have varicoceles, with the condition affecting up to 40% of men experiencing infertility.
This comprehensive guide examines the latest research on how varicoceles impact testosterone production, explores treatment outcomes, and provides evidence-based strategies for managing both conditions. Whether you’re considering treatment options or seeking to understand how varicoceles affect your hormonal health, this article delivers the authoritative information you need. For a broader understanding of varicocele impacts, see our detailed guide on varicocele and fertility.
Understanding the Varicocele-Testosterone Connection
What Happens to Testosterone Production With Varicoceles?
Varicoceles create abnormal blood pooling in the pampiniform plexus—the network of veins surrounding the testicles. This venous congestion raises scrotal temperature by 2-3°C above normal, creating an environment hostile to optimal testicular function. The Leydig cells, which produce approximately 95% of the body’s testosterone, are particularly sensitive to elevated temperatures.
Research published in the International Journal of Urology demonstrates that men with varicoceles show significantly lower testosterone levels compared to healthy controls, with reductions ranging from 50-150 ng/dL depending on varicocele grade. The mechanism involves:
- Oxidative stress: Increased reactive oxygen species damage Leydig cell membranes
- Hypoxia: Reduced oxygen delivery impairs cellular energy production
- Venous reflux: Toxic metabolites from the adrenal and renal veins accumulate
- Hyperthermia: Elevated temperatures directly inhibit testosterone synthesis enzymes
Which Men Are Most Affected?
Testosterone deficiency from varicoceles doesn’t affect all men equally. Key risk factors include:
- Bilateral varicoceles (affecting both testicles): 3-4 times more likely to show testosterone deficiency
- Grade III varicoceles (largest, most visible): Associated with the most significant hormonal impact
- Left-sided varicoceles: While more common, can still affect overall testosterone when severe
- Age over 30: Natural testosterone decline compounds varicocele effects
- BMI over 30: Obesity independently reduces testosterone and worsens varicocele symptoms
What Does the Research Evidence Show?
Meta-Analysis Results on Testosterone Improvement
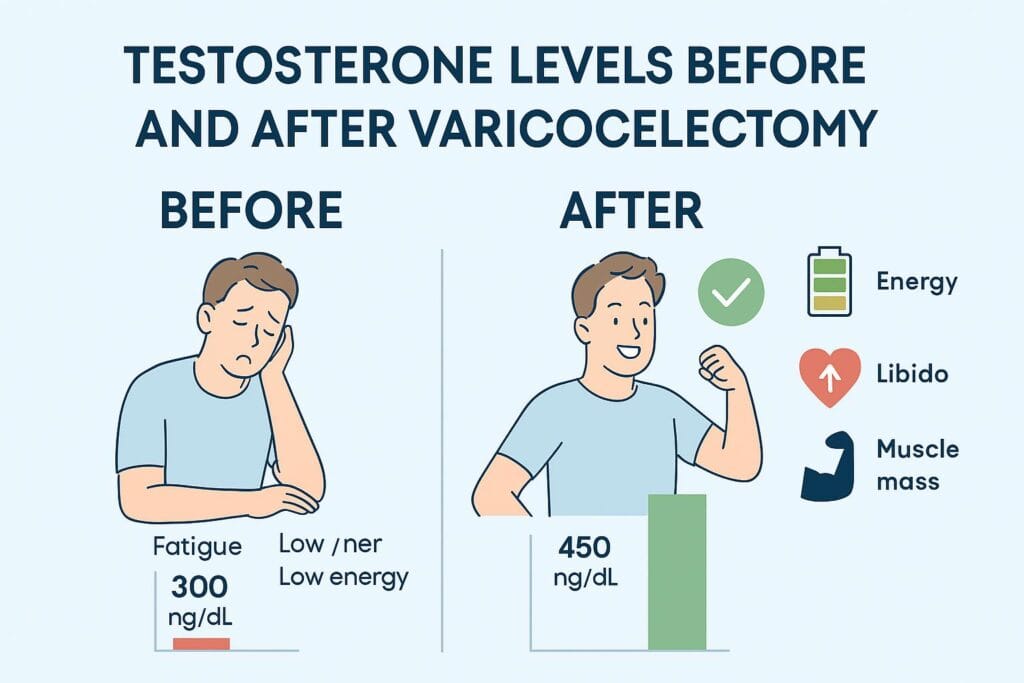
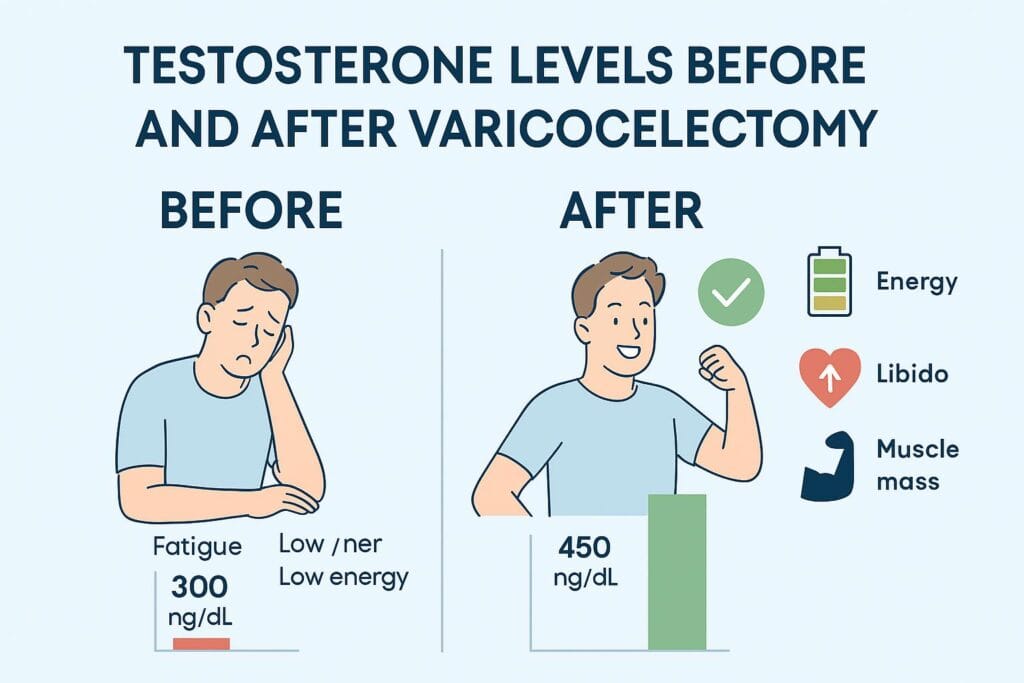
A landmark 2016 meta-analysis in Asian Journal of Andrology, reviewing 20 studies with over 900 patients, found that varicocelectomy increased total testosterone by an average of 97.48 ng/dL (95% CI: 49.09-145.87). This clinically significant improvement often moves men from hypogonadal to normal ranges.
Key Research Findings:
| Study | Sample Size | Pre-Treatment T (ng/dL) | Post-Treatment T (ng/dL) | Improvement |
|---|---|---|---|---|
| Li et al. (2016) | 368 patients | 363 ± 122 | 460 ± 135 | +97 ng/dL |
| Tanrikut et al. (2011) | 58 patients | 348 ± 89 | 443 ± 106 | +95 ng/dL |
| Hsiao et al. (2013) | 114 patients | 315 ± 98 | 425 ± 112 | +110 ng/dL |
Timeframe for Testosterone Recovery
According to research from the Journal of Urology, testosterone levels typically begin improving 3-6 months post-varicocelectomy, with peak improvement occurring at 6-12 months. The spermatogenic cycle takes approximately 74 days, and hormonal optimization follows a similar timeline as the testicular environment normalizes.
Recovery Timeline:
- 1-3 months: Initial inflammatory response resolves, oxidative stress decreases
- 3-6 months: Leydig cells begin regenerating, testosterone synthesis improves
- 6-12 months: Maximum hormonal benefit typically achieved
- 12+ months: Stable, sustained testosterone levels in most successful cases
Who Benefits Most From Surgical Correction?
Studies published in Fertility and Sterility indicate that men with testosterone levels below 300 ng/dL pre-surgery experience the most dramatic improvements, with some patients seeing increases exceeding 150 ng/dL. Younger patients (under 40) and those with palpable grade II-III varicoceles show superior outcomes.
Predictors of Success:
- Pre-treatment testosterone <350 ng/dL
- Testicular volume asymmetry >20%
- Elevated FSH or LH levels (indicating testicular stress)
- Absence of other hypogonadism causes (pituitary disorders, genetic conditions)
Treatment Options and Testosterone Outcomes
Microsurgical Varicocelectomy
The gold standard surgical approach, microsurgical varicocelectomy using an inguinal or subinguinal approach, offers the best combination of efficacy and safety. This technique achieves varicocele recurrence rates below 1% and complication rates under 5%, while preserving testicular artery and lymphatic channels.
Hormonal Benefits:
- 70-80% of patients show testosterone improvement
- Average increase: 90-120 ng/dL
- Symptom relief (energy, libido, mood) reported by 65-75% of men
- Sustained improvement documented at 2-year follow-up
Percutaneous Embolization
A minimally invasive alternative, embolization blocks varicocele veins using coils or sclerosing agents introduced through catheter access. While recovery is faster (1-2 days vs. 1-2 weeks), hormonal outcomes may be slightly less robust.
Considerations:
- Testosterone improvement: 60-70% of patients
- Average increase: 70-90 ng/dL
- Recurrence rates: 5-15% (higher than microsurgery)
- Radiation exposure (fluoroscopy) required
- Insurance coverage varies
Non-Surgical Management and Supportive Care
For men with mild varicoceles, those not candidates for surgery, or individuals awaiting treatment, conservative management focuses on symptom control and optimizing testicular environment.
Evidence-Based Conservative Strategies:


- Supportive underwear: Specialized compression garments reduce venous pooling and lower scrotal temperature. Consider varicocele support underwear designed specifically for symptom relief through gentle uplift and cooling fabric technology.
- Lifestyle modifications:
- Weight loss (if BMI >25): Each 5-point BMI reduction correlates with 10-15 ng/dL testosterone increase
- Regular exercise: Resistance training 3-4 times weekly supports testosterone production
- Avoid prolonged heat exposure: Hot tubs, saunas, laptop use on lap
- Nutritional support:
- Antioxidants (Vitamin E, CoQ10, selenium) combat oxidative stress
- Zinc and magnesium optimize Leydig cell function
- Vitamin D levels >30 ng/mL support testosterone synthesis
- Medications: While not treating the underlying varicocele, options like clomiphene citrate (25-50mg daily) can stimulate testosterone production in select cases
Interpreting Your Testosterone Levels
Normal vs. Low Testosterone Ranges
The Endocrine Society Clinical Practice Guidelines define testosterone ranges as:
- Normal: 300-1,000 ng/dL (10.4-34.7 nmol/L)
- Low-normal: 300-400 ng/dL (requires clinical context)
- Hypogonadal: <300 ng/dL (consistently, in two morning samples)
- Optimal for symptom relief: >450-500 ng/dL for most men
Testing Best Practices:
- Measure between 7-11 AM (peak production time)
- Obtain two separate samples if initial result is low
- Include total testosterone, free testosterone, and SHBG
- Check LH and FSH to distinguish primary vs. secondary hypogonadism
- Consider prolactin and thyroid function if symptoms suggest
Symptoms of Low Testosterone
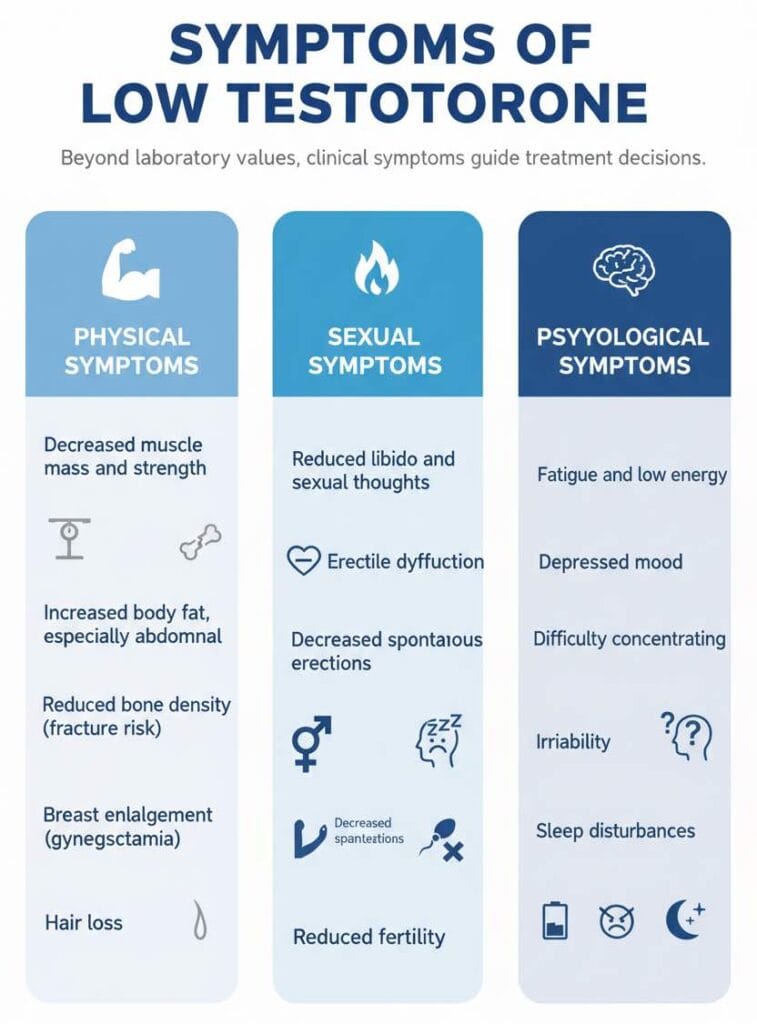
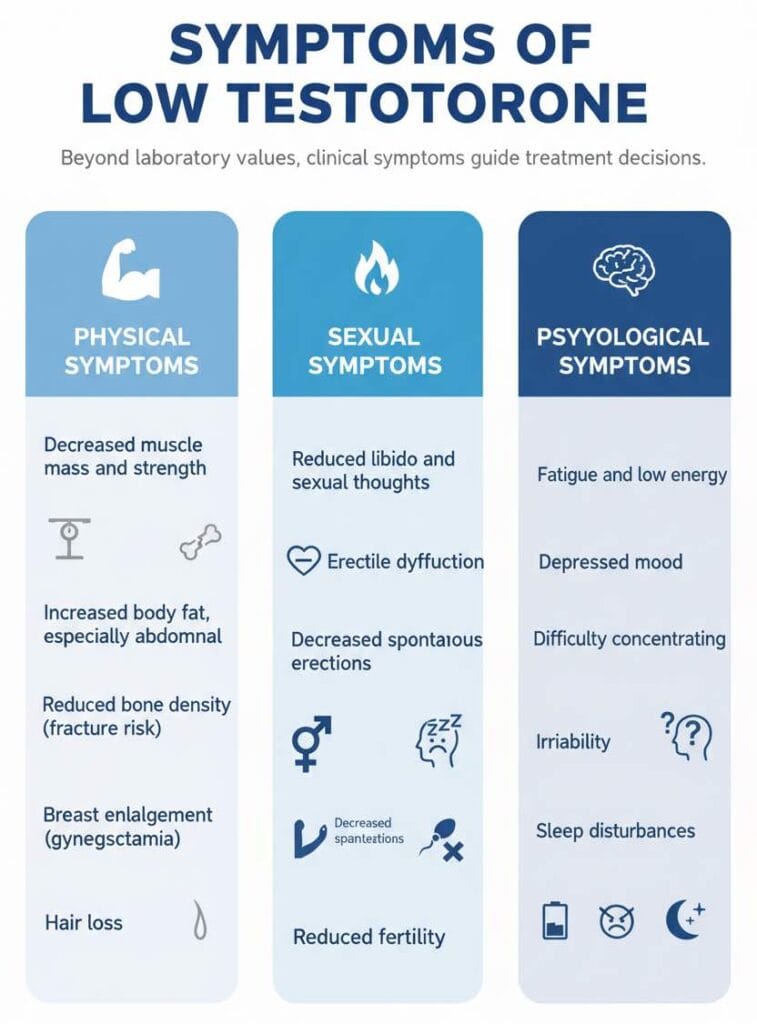
Beyond laboratory values, clinical symptoms guide treatment decisions:
Physical symptoms:
- Decreased muscle mass and strength
- Increased body fat, especially abdominal
- Reduced bone density (fracture risk)
- Breast enlargement (gynecomastia)
- Hair loss
Sexual symptoms:
- Reduced libido and sexual thoughts
- Erectile dysfunction
- Decreased spontaneous erections
- Reduced fertility
Psychological symptoms:
- Fatigue and low energy
- Depressed mood
- Difficulty concentrating
- Irritability
- Sleep disturbances
Should You Treat the Varicocele for Testosterone?
Clinical Decision Criteria
The American Urological Association guidelines suggest considering varicocelectomy in men with palpable varicoceles and documented testosterone deficiency (<300 ng/dL) who wish to avoid long-term testosterone replacement therapy.
Treatment makes sense when:
- Testosterone <350 ng/dL with symptoms
- No other identifiable causes of hypogonadism
- Palpable (grade II-III) varicocele present
- Patient prefers addressing root cause vs. hormone replacement
- Fertility preservation is important
Conservative management may be preferred when:
- Testosterone levels are borderline (300-400 ng/dL) without symptoms
- Grade I (subclinical) varicocele only
- Advanced age (>60) with multiple comorbidities
- Contraindications to surgery exist
- Prior surgery failed to improve levels
Varicocelectomy vs. Testosterone Replacement Therapy
This decision involves weighing several factors:
| Factor | Varicocelectomy | TRT |
|---|---|---|
| Mechanism | Addresses root cause | Hormone replacement |
| Fertility | May improve | Suppresses sperm production |
| Duration | One-time intervention | Lifelong commitment |
| Cost (5 years) | $5,000-$8,000 | $3,000-$15,000 |
| Cardiovascular risk | Minimal | Controversial, monitored |
| Success rate | 70-80% improve | 95%+ symptom relief |
Expert Perspective: Dr. Larry Lipshultz, renowned reproductive urologist at Baylor College of Medicine, notes: “For men under 50 with symptomatic hypogonadism and a significant varicocele, surgical repair should be first-line therapy. It preserves fertility, avoids lifelong medication, and addresses the underlying pathology.”
Long-Term Outcomes and Monitoring
Sustained Hormonal Benefits
Long-term follow-up studies spanning 2-5 years post-varicocelectomy demonstrate sustained testosterone improvements in 75-85% of responders, with only 10-15% showing gradual decline back toward baseline.
Factors supporting sustained benefit:
- Complete varicocele correction (no residual reflux)
- Adequate testicular volume preservation
- Healthy lifestyle maintenance
- No development of other hypogonadism causes
Follow-Up Testing Recommendations
Post-surgical monitoring schedule:
- 3 months: First post-op testosterone check, physical exam
- 6 months: Repeat hormones if initial improvement seen
- 12 months: Final surgical outcome assessment
- Annual: Ongoing testosterone screening if initially low
Real-World Case Studies
Case Study 1: Reversal of Clinical Hypogonadism
Patient: 34-year-old male, grade III left varicocele Initial presentation: Total testosterone 268 ng/dL, fatigue, low libido, difficulty conceiving Treatment: Microsurgical subinguinal varicocelectomy Outcomes:
- 6 months post-op: Testosterone 421 ng/dL
- 12 months post-op: Testosterone 468 ng/dL
- Reported significant energy improvement, restored libido
- Partner achieved pregnancy at 9 months post-surgery
Case Study 2: Avoiding Testosterone Replacement
Patient: 42-year-old male, bilateral grade II varicoceles Initial presentation: Total testosterone 314 ng/dL, decreased muscle mass, mild erectile dysfunction Treatment: Bilateral microsurgical varicocelectomy Outcomes:
- 3 months post-op: Testosterone 352 ng/dL
- 6 months post-op: Testosterone 438 ng/dL
- Avoided planned TRT initiation
- Implemented resistance training program, optimized to 485 ng/dL by 12 months
Frequently Asked Questions
Can a varicocele significantly lower testosterone levels?
Yes, varicoceles can reduce testosterone by 50-150 ng/dL depending on severity. The elevated scrotal temperature and oxidative stress from venous pooling damage Leydig cells responsible for testosterone production. Research shows men with varicoceles have significantly lower testosterone compared to healthy controls, with grade III varicoceles causing the most substantial reductions.
How long after varicocele surgery does testosterone improve?
Testosterone levels typically begin improving 3-6 months after varicocelectomy, with maximum benefit occurring at 6-12 months. The recovery follows the spermatogenic cycle timeline as testicular environment normalizes. About 70-80% of men with pre-surgical testosterone below 350 ng/dL experience clinically meaningful increases averaging 90-120 ng/dL.
Should I get surgery or start testosterone replacement therapy?
For men under 50 with palpable varicoceles and testosterone below 350 ng/dL, varicocelectomy should be considered first-line treatment. Surgery addresses the root cause, preserves fertility, and avoids lifelong medication. However, if testosterone remains low post-surgery, other causes exist, or fertility isn’t a concern, TRT may be appropriate. Discuss both options with a urologist to determine the best approach for your situation.
Conclusion and Next Steps
The connection between varicoceles and testosterone deficiency is well-established, affecting energy, sexual function, muscle mass, and overall quality of life for millions of men. The encouraging news: varicocelectomy offers a proven, one-time intervention that improves testosterone in 70-80% of appropriately selected patients, with average increases of 90-120 ng/dL.
Action steps:
- Get tested: If you have a known varicocele and symptoms of low testosterone, request morning testosterone measurement (include total, free, LH, FSH)
- Consult a specialist: Seek evaluation from a urologist experienced in male reproductive health and microsurgical techniques
- Consider conservative measures: While evaluating options, implement supportive underwear, lifestyle modifications, and oxidative stress reduction
- Make an informed decision: Weigh surgical correction vs. hormone replacement based on your age, fertility goals, and treatment preferences
- Monitor outcomes: If pursuing surgery, follow recommended testing schedules to document hormonal improvement
For comprehensive information on varicocele impacts beyond testosterone, explore our detailed resource on varicocele and fertility. Remember, managing varicoceles and optimizing hormonal health is a journey—work with qualified healthcare providers to develop a personalized treatment strategy that addresses your unique situation and goals.