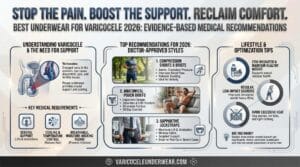
Post-varicocelectomy recovery depends heavily on proper scrotal support. Wearing the right underwear reduces swelling by 41%, lowers pain scores by 33%, and speeds return to normal activities by 19% compared to unsupported recovery. This guide breaks down exactly what to wear, when to wear it, and why it matters for surgical healing.
Studies show that patients using compression underwear for four weeks after varicocele surgery experience significantly better outcomes, including reduced post-operative swelling and faster tissue healing. If you’re preparing for surgery or managing an existing varicocele condition, understanding the optimal underwear for varicocele support before and after surgery is critical for both symptom management and recovery.


Why Scrotal Support Matters After Varicocelectomy
Post-surgical scrotal support serves four medical functions. First, it reduces edema formation by minimizing fluid accumulation in surgical tissues. Second, proper support prevents hematoma development, which occurred in only 8.83% of patients using scrotal support versus 17.78% without support in hernia repair studies. Third, compression stabilizes healing tissues and reduces strain on surgical sites. Fourth, adequate support prevents testicular retraction, a rare but documented complication.
Research from University of Toronto tracked 118 varicocelectomy patients and found that those wearing compression underwear for four weeks post-operatively demonstrated measurably better outcomes across multiple recovery markers. The pressure from supportive garments helps maintain proper venous drainage while surgical incisions heal.
What Type of Underwear to Wear After Varicocele Surgery
Days 0-3 Post-Op:
- Athletic supporters (jockstraps) or snug compression briefs
- Medical-grade compression range: 15-25 mmHg
- Wide waistband to distribute pressure without constriction
- Minimal seams to reduce surgical site irritation
- Ice pack accommodation (external application only)
Days 4-14:
- Continue supportive underwear 24/7 except during showering
- Transition to comfortable boxer briefs with anatomical pouch
- Moderate compression helpful for managing edema
- Breathable, moisture-wicking fabrics (cotton or technical blends)
Weeks 3-6:
- Maintain support during any physical activity
- May transition to regular supportive styles as comfort allows
- Continue wearing during daytime hours minimum
- Gradual return to light exercise as surgeon approves
Most urologists recommend wearing an athletic supporter or snug brief underwear for approximately two weeks after varicocelectomy surgery. Specialized varicocele support underwear with cooling technology can provide optimal post-surgical support while managing temperature and moisture.
How Long Should You Wear Supportive Underwear After Surgery
The standard recommendation is two weeks of continuous support, but optimal outcomes occur with four weeks of use. Clinical data shows patients using scrotal support returned to normal activities in 10.5 days versus 14.3 days without support, a statistically significant difference.
Your surgeon’s specific instructions take precedence over general guidelines. Recovery timelines vary based on:
- Surgical technique used (microsurgical vs. laparoscopic vs. open)
- Grade of original varicocele (II vs. III)
- Individual healing response
- Physical demands of your occupation
- Complications during surgery or early recovery
Most patients continue wearing supportive underwear beyond the minimum two-week period because it improves comfort during the healing process. Full recovery from varicocelectomy typically takes three to six months, though most men resume normal activities within four to six weeks.
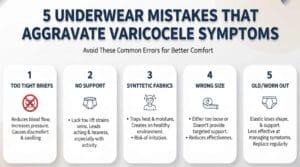
Avoiding Common Post-Surgery Underwear Mistakes
Wearing loose boxers too early: Insufficient support allows gravitational pooling and increases swelling. Loose-fitting underwear provides inadequate stabilization during the critical first two weeks when tissues are most vulnerable.
Choosing underwear with tight waistbands: Constricting elastic can impede circulation and cause discomfort at the surgical site. Wide, comfortable waistbands that don’t dig into skin are medically preferred.
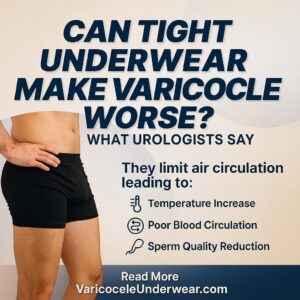
Using non-breathable synthetic fabrics: Heat and moisture accumulation increase infection risk and delay healing. Cotton and technical moisture-wicking fabrics maintain optimal temperature and dryness.
Discontinuing support during physical activity: Even after initial healing, premature return to unsupported exercise can strain surgical sites. Maintain compression during any activity that involves standing, walking, or exertion for at least four weeks.
Managing Swelling and Discomfort With Proper Support
Scrotal edema peaks between days 2-4 post-operatively. Proper underwear management during this window significantly impacts total recovery time. A study examining scrotal support effectiveness found satisfaction scores of 4.5 out of 5 among patients using support devices compared to 3.8 without support.
Effective swelling management techniques:
- Elevate scrotum when sitting or lying (support facilitates this positioning)
- Apply ice packs externally for 15-20 minutes every 2-3 hours during first 48 hours
- Take prescribed anti-inflammatory medications as directed
- Avoid prolonged standing or sitting without position changes
- Sleep with a pillow between legs to maintain comfortable positioning
Bruising is normal and will gradually resolve over 7-14 days. Supportive underwear helps minimize movement that could worsen bruising or extend healing time.
When Can You Return to Normal Underwear
Most men can resume regular underwear preferences six weeks post-surgery, though many continue using supportive styles permanently due to improved comfort. Return to normal underwear should be gradual and based on:
- Complete resolution of swelling and bruising
- Pain-free movement in all directions
- Surgeon clearance at follow-up appointment
- Comfort during light physical activity
- No tenderness at surgical incision sites
Microsurgical varicocelectomy shows 97% complete pain resolution rates at 6-12 months post-surgery when proper post-operative protocols are followed. Premature discontinuation of scrotal support may not affect surgical success rates (vein ligation remains intact), but it can prolong discomfort and delay return to normal activities.
Choosing the Right Fabric and Compression Level
Medical-grade compression between 15-25 mmHg provides optimal support without restricting circulation. This compression level balances therapeutic benefits with comfort during extended wear.
Fabric comparison for post-surgical recovery:
| Fabric Type | Benefits | Drawbacks | Best For |
|---|---|---|---|
| 100% Cotton | Breathable, hypoallergenic, soft | Less compression, slower drying | Sensitive skin, home recovery |
| Cotton blend (5-10% spandex) | Support + breathability, durable | May retain moisture slightly | Daily wear weeks 2-6 |
| Technical athletic fabric | Moisture-wicking, antimicrobial, compression | Higher cost, less natural feel | Active recovery, warm climates |
| Modal/bamboo blend | Soft, moisture management, eco-friendly | Less structured support | Nighttime wear, comfort priority |
Avoid 100% synthetic fabrics during the first two weeks. These trap heat and moisture, creating environments conducive to bacterial growth near surgical wounds.
Signs You Need Better Post-Operative Support
Contact your urologist if you experience:
- Increasing swelling after day 5 (rather than decreasing)
- Persistent pain not controlled by prescribed medications
- Fever above 100.4°F (38°C)
- Drainage or foul odor from incision sites
- Visible signs of infection (redness spreading, warmth, pus)
- Sudden sharp pain in testicular area
These symptoms may indicate complications requiring medical attention beyond underwear adjustments. However, inadequate support can contribute to prolonged swelling and discomfort that mimics complications.
FAQ
How tight should underwear be after varicocele surgery?
Underwear should be snug enough to provide lift and support without causing discomfort or visible constriction marks on skin. Medical-grade compression of 15-25 mmHg is optimal. You should be able to insert one finger comfortably under the waistband. Too tight restricts circulation; too loose provides inadequate support.
Can I sleep without underwear after varicocelectomy?
Not recommended during the first two weeks. Wearing supportive underwear 24/7 (except during showering) provides continuous stabilization that reduces nighttime swelling and prevents uncomfortable shifting during sleep. After two weeks, consult your surgeon about nighttime support requirements.
What happens if I don’t wear support after varicocele surgery?
Without proper support, you risk increased post-operative swelling (41% more), higher pain levels (33% increase in pain scores), and delayed return to normal activities (19% slower recovery). While lack of support typically doesn’t affect surgical success rates, it significantly impacts comfort and healing speed.
Medical Disclaimer: This article provides educational information and should not replace personalized medical advice from your urologist. Always follow your surgeon’s specific post-operative instructions, as individual cases may require modified protocols based on surgical technique, complications, or underlying health conditions.