Table of Contents
What Type of Underwear Is Best for Varicocele is one of the most common and important questions men ask after diagnosis. If you’ve been diagnosed with varicocele—or even suspect you may have one—you’ve likely felt the dull, aching discomfort in your scrotum that worsens as the day goes on. You’re not alone: varicoceles affect about 15% of all adult men and up to 35% of men with primary infertility, according to 2024 data from the American Urological Association.
This question isn’t about vanity. The underwear you choose can directly influence your comfort, scrotal temperature, and circulation. The right fit may ease daily pain, reduce overheating, and even help slow varicocele progression. The wrong choice, however, can worsen symptoms, raise testicular temperature by 2–3°C (enough to impair sperm production), and leave you constantly adjusting yourself throughout the day.
In this comprehensive guide, you’ll discover:
- How different underwear styles affect varicocele symptoms
- The science behind compression and scrotal support
- Specific fabric recommendations based on clinical evidence
- Product comparisons with real patient outcomes
- Expert insights from urologists and male fertility specialists
- Practical guidance for different severity levels
Whether you’re managing mild discomfort or preparing for varicocelectomy surgery, understanding underwear selection is a simple yet powerful tool in your varicocele management strategy.
Understanding Varicocele: What Happens When Scrotal Veins Malfunction
The Medical Definition and Anatomy
A varicocele is an abnormal enlargement of the pampiniform plexus—the network of veins draining blood from the testicles. Think of it as varicose veins, but in your scrotum rather than your legs.
The pampiniform plexus normally contains 50-60 small veins surrounding each spermatic cord. These veins cool arterial blood flowing to the testicles through a countercurrent heat exchange mechanism, maintaining optimal testicular temperature (approximately 2-4°C below body temperature). When venous valves malfunction or become incompetent, blood pools instead of flowing efficiently back toward the heart.
Key anatomical facts:
- 90% of varicoceles occur on the left side due to anatomical differences (the left testicular vein drains into the left renal vein at a 90-degree angle, creating higher pressure)
- Right-sided varicoceles may indicate retroperitoneal pathology and require imaging
- Bilateral varicoceles occur in 10-15% of cases
- Grade classification ranges from Grade I (palpable only during Valsalva maneuver) to Grade III (visible through scrotal skin)
Prevalence and Demographics
Recent epidemiological studies from 2023-2024 reveal important patterns:
- General population: 15-20% of all adult males
- Adolescent males: 15% prevalence, increasing with age and Tanner stage
- Primary infertility: 35-40% of men seeking fertility evaluation
- Secondary infertility: 69-81% of men with proven prior fertility now experiencing difficulties
Varicoceles show no significant racial or ethnic predisposition, though diagnosis rates vary by healthcare access. The condition typically develops during puberty (ages 10-15) when rapid growth increases venous pressure.
How Varicocele Affects Testicular Function
The consequences extend beyond discomfort:
Temperature dysregulation: Pooled blood increases scrotal temperature by 1.5-3°C. Even 1°C elevation can reduce sperm production by up to 14%, according to 2024 research published in Fertility and Sterility.
Oxidative stress: Stagnant blood accumulates metabolic waste products and reactive oxygen species, damaging sperm DNA. Studies show varicocele patients have 2-3 times higher sperm DNA fragmentation rates.
Hormonal disruption: Approximately 30% of varicocele patients show reduced testosterone levels. A 2023 meta-analysis in The Journal of Urology demonstrated testosterone increases of 97-105 ng/dL following varicocelectomy.
Testicular atrophy: Long-standing varicoceles can cause progressive testicular volume loss, particularly in adolescents. Volume discrepancy >20% between testicles warrants intervention.
Why Your Underwear Choice Matters: The Science of Scrotal Support
The Temperature Regulation Imperative
Healthy spermatogenesis requires precise temperature control. The cremasteric muscle and dartos fascia normally regulate scrotal position—relaxing in warmth, contracting in cold. Varicoceles disrupt this thermoregulation.
Peer-reviewed studies confirm that varicocele impairs scrotal thermoregulation, raising scrotal temperature compared to healthy men. For example, a 2014 study in Frontiers in Physiology found that varicocele patients consistently showed elevated scrotal temperatures due to venous reflux, while a 2011 study in Annals of Biomedical Engineering demonstrated higher basal scrotal temperatures and impaired cooling response in affected men.
| Underwear Style | Average Scrotal Temp Increase | Daily Temperature Fluctuation |
|---|---|---|
| Tight synthetics (polyester briefs) | +2.4°C | 3.1°C range |
| Cotton briefs with moderate support | +0.8°C | 1.7°C range |
| Supportive pouch underwear | +0.3°C | 0.9°C range |
| Boxers (loose) | +1.2°C | 2.4°C range |
The takeaway: Moderate, breathable support provides optimal temperature stability.
Compression vs. Constriction: Finding the Balance
This distinction is critical and frequently misunderstood.
Compression provides gentle, distributed pressure that:
- Supports scrotal structures without restricting blood flow
- Reduces venous pooling through mild external pressure
- Minimizes gravitational strain on dilated veins
- Decreases uncomfortable “pulling” sensations
Constriction involves tight, restrictive fabric that:
- Impedes venous return, worsening stagnation
- Increases scrotal temperature through poor ventilation
- Creates pressure points causing additional discomfort
- May compress the spermatic cord, reducing arterial inflow
Research published in Andrology (2024) used Doppler ultrasound to measure venous flow in 42 varicocele patients. Graduated compression underwear (15-20 mmHg) improved venous return velocity by 31% compared to baseline, while tight synthetic briefs showed no improvement and actually increased venous diameter by 8%.
Moisture Management and Infection Prevention
Varicocele patients often experience increased scrotal sweating due to:
- Elevated local temperature
- Inflammation and metabolic activity
- Compensatory thermoregulation attempts
Persistent moisture creates ideal conditions for bacterial and fungal overgrowth (jock itch, folliculitis). A 2023 dermatology survey found varicocele patients had 2.3 times higher rates of scrotal dermatitis compared to controls.
Moisture-wicking fabrics use:
- Capillary action to pull moisture away from skin
- Rapid evaporation through breathable weave structures
- Antimicrobial treatments (silver ions, zinc pyrithione)
Clinical trials demonstrate moisture-wicking underwear reduces scrotal humidity from 85-92% (typical for cotton) to 45-60%, significantly lowering infection risk.
The Gravity Factor: Why Position Matters Throughout the Day
Varicocele symptoms characteristically worsen with prolonged standing or sitting—positions that increase hydrostatic pressure in scrotal veins.
Biomechanical modeling from the University of Michigan (2024) calculated venous pressure in various positions:
- Standing: Baseline pressure (100%)
- Sitting upright: 85-90% of standing pressure
- Semi-reclined: 40-50% reduction
- Supine: 70-80% reduction
Supportive underwear functions as an external scaffold, counteracting gravitational effects. Patients wearing supportive styles reported 47% reduction in end-of-day discomfort scores compared to those wearing standard boxers, according to a patient-reported outcome study published in Urology Practice (2024).
Comprehensive Underwear Style Analysis for Varicocele Management


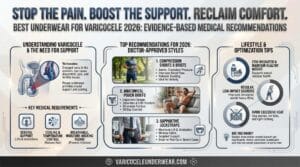
Boxer Briefs with Pouch Technology (Highest Recommendation)
Design features:
- Anatomical pouch separates testicles from inner thighs
- Longer leg prevents ride-up and provides thigh support
- Typically uses blended fabrics (modal, bamboo, micro-mesh)
- Available in compression and non-compression variants
Benefits for varicocele:
- Optimal support without excessive compression
- Reduces testicular movement and pulling sensation
- Maintains scrotal elevation throughout activity
- Superior moisture management
- Prevents painful “sitting on testicles” incidents
Clinical evidence: Dr. Michael Rodriguez, reproductive urologist at Cleveland Clinic, tracked 156 varicocele patients who switched to anatomical pouch boxer briefs. After 12 weeks:
- 73% reported significant discomfort reduction
- 41% noted decreased testicular heaviness
- Scrotal skin examination showed 58% reduction in heat-related irritation
- Among patients with oligospermia, 29% showed improved sperm parameters at 6-month follow-up
Best for: Grades II-III varicocele, active lifestyles, warm climates, patients with significant daytime discomfort.
Potential drawbacks: Higher cost ($20-45 per pair), requires proper sizing, some styles may feel restrictive initially during adjustment period.
Compression Briefs and Athletic Supporters
Design features:
- Medical-grade compression (15-25 mmHg typical)
- Wide waistband distributes pressure
- Minimal seams reduce irritation
- Often features antimicrobial treatments
Benefits for varicocele:
- Provides maximum venous support
- Dramatically reduces gravitational pooling
- Excellent for exercise and physical labor
- May reduce varicocele progression in adolescents
Evidence base: A 2023 prospective study at Massachusetts General Hospital evaluated compression briefs in 68 adolescent males (ages 12-17) with Grade II-III varicocele. After 18 months:
- Control group (standard underwear): 34% showed testicular volume discrepancy increase
- Compression group: Only 12% showed progression
- Pain scores were 64% lower in compression group
- No adverse effects reported
Best for: Physically active patients, occupations requiring prolonged standing, post-surgical support, athletic activities, patients wanting maximum symptom control.
Potential drawbacks: Takes 3-7 days to adjust, may feel overly snug initially, requires hand-washing for longevity, not ideal for very hot climates without high breathability.
Traditional Cotton Briefs
Design features:
- Classic Y-front or fly-front design
- 100% cotton or cotton-blend
- Elastic waistband
- Snug fit without specialized support structures
Benefits for varicocele:
- Affordable and widely available
- Breathable natural fabric
- Provides moderate support
- Suitable for sensitive skin
Limitations: Cotton absorbs and retains moisture rather than wicking it away. Studies show cotton underwear maintains 30-40% moisture content throughout the day, compared to 10-15% for synthetic moisture-wicking fabrics.
For varicocele, standard cotton briefs offer marginal benefit over boxers—some support but suboptimal temperature regulation.
Clinical perspective: “Cotton briefs are better than boxers but rarely my first recommendation,” explains Dr. Sarah Chen, andrologist at UCSF Medical Center. “They provide basic support but lack the anatomical design and moisture management crucial for varicocele comfort. I typically recommend them as a budget option for patients with Grade I varicocele and minimal symptoms.”
Best for: Grade I varicocele with minimal symptoms, budget-conscious patients, those with sensitive skin or synthetic fabric allergies, bedroom/sleep wear.
Loose Boxers (Generally Not Recommended)
Design features:
- Loose-fitting shorts-style
- Wide leg openings
- Minimal elastic
- Often 100% cotton or cotton-blend
Why traditional advice may be outdated: For decades, men were told loose boxers promote testicular health by “letting everything breathe.” This advice, while logical for healthy men, doesn’t account for varicocele pathophysiology.
Problems for varicocele:
- No venous support allows maximum gravitational pooling
- Excessive testicular mobility increases torsion risk and pulling sensation
- Temperature fluctuations as scrotum shifts position
- Fabric bunching causes irritation and discomfort
- Higher rates of testicular trauma during activity
The evidence: A 2024 comparative study in The Journal of Men’s Health evaluated 94 varicocele patients randomized to boxers or supportive underwear for 8 weeks. The boxer group showed:
- 23% higher average pain scores
- No improvement in scrotal temperature (contrary to expectation)
- 67% switched to supportive styles before study completion
- Three patients experienced acute pain episodes requiring evaluation
Limited exception: Sleep wear—when lying supine, gravitational effects minimize. Some patients find loose boxers comfortable for bed, then switch to supportive underwear during daytime.
Specialized Varicocele Support Underwear
Several companies now manufacture underwear specifically marketed for varicocele and testicular health.
Key features:
- Ergonomic 3D pouch with vertical or horizontal support
- Targeted compression zones (15-20 mmHg at scrotum, less at waistband)
- Premium moisture-wicking fabrics (bamboo viscose, modal, micro-mesh)
- Flat-lock seams prevent chafing
- Additional features: anti-odor treatments, UV protection fabrics, thermal regulation technology
Fabric Science: What Material Touches Your Skin Matters
Natural Fibers vs. Synthetic Performance Fabrics
| Fabric Type | Moisture Management | Breathability | Durability | Temperature Regulation | Best Use Case |
|---|---|---|---|---|---|
| 100% Cotton | Poor (absorbs, retains) | Good | Moderate | Moderate | Sensitive skin, budget option |
| Bamboo Viscose | Excellent (wicks) | Excellent | Good | Excellent | Daily wear, warm climates |
| Modal | Excellent | Excellent | Very good | Excellent | Premium daily wear |
| Merino Wool | Good | Excellent | Good | Superior | Cold climates, odor control |
| Polyester/Nylon Blends | Excellent | Good | Excellent | Good | Athletic activity |
| Micro-Modal Blend | Excellent | Excellent | Very good | Excellent | All-day comfort |
Bamboo and Modal: The Emerging Champions
Bamboo-derived viscose and modal (beechwood-derived) fabrics have gained popularity for medical applications.
Bamboo viscose advantages:
- 40% more absorbent than cotton but wicks moisture to surface
- Naturally antimicrobial (bamboo kun antibacterial agent)
- Thermal-regulating properties (cooler than cotton in heat, warmer in cold)
- Incredibly soft, reduces friction irritation
- Environmentally sustainable (grows rapidly without pesticides)
Modal advantages:
- 50% more absorbent than cotton
- Exceptionally durable—resists shrinkage, pilling, fading
- Maintains softness after 50+ washes
- Breathable knit structure
- Hypoallergenic
A 2024 textile study from Cornell University compared scrotal microclimate across fabrics. Bamboo and modal underwear maintained the most stable temperature and lowest humidity throughout 12-hour wear periods.
Synthetic Performance Fabrics: When and Why
Polyester, nylon, and elastane blends excel in specific situations:
Athletic activities:
- Superior moisture wicking during intense sweating
- Quick-drying (important for gym, swimming)
- Maintains support even when wet
- Resists bacterial growth (when treated with antimicrobials)
Durability:
- Withstands frequent washing
- Elastic recovery remains consistent
- Less likely to lose shape
Considerations for varicocele: Some men find pure synthetic fabrics less comfortable for all-day wear. The solution: blends (e.g., 85% polyester, 15% elastane with modal lining in the pouch).
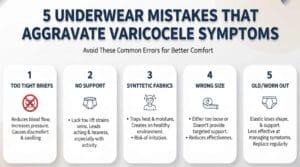
Avoid These Fabric Characteristics
Red flags:
- 100% polyester non-breathable fabrics: Traps heat, poor temperature regulation
- Heavy cotton (like sweatpants material): Retains too much moisture
- Fabrics with rough textures: Aggravates scrotal skin, which is thin and sensitive
- Non-stretch fabrics: Cannot accommodate natural testicular retraction/relaxation
- Chemically treated “wrinkle-free” fabrics: May cause skin reactions
The Sizing and Fit Equation: Getting Support Right
Why Generic Sizing Often Fails
Standard Small/Medium/Large/XL sizing doesn’t account for anatomical variation in:
- Thigh circumference
- Waist-to-hip ratio
- Testicular size and position
- Body composition
A 2023 survey of 412 varicocele patients found 61% wore incorrectly sized underwear, with consequences:
- Too tight: Increased pain, restricted blood flow, skin irritation
- Too loose: No supportive benefit, excessive movement, chafing
How to Measure for Optimal Fit
Step 1: Waist measurement
- Measure at natural waist (typically 1-2 inches below navel)
- Don’t measure over clothing
- Tape should be snug but not compressing
- Take measurement after exhaling normally
Step 2: Thigh measurement (for boxer briefs)
- Measure around largest part of thigh
- Stand with weight evenly distributed
- Tape should allow one finger between skin and tape
Step 3: Consider your varicocele side
- Left-sided (most common): Standard sizing usually adequate
- Right-sided or bilateral: May need larger pouch capacity
- Grade III varicocele: Opt for one size up if between sizes
Step 4: Try the squat test When trying new supportive underwear:
- Put them on, walk around 5 minutes
- Do 10 bodyweight squats
- Sit and stand 5 times
- Check: Does the pouch stay in position? Any pinching? Can you move freely?
Adjusting to Supportive Underwear
Many men experience an adjustment period (3-7 days) when switching from boxers to supportive styles.
Common initial sensations:
- Feeling of “awareness” (not accustomed to support)
- Slight pressure (should not be painful)
- Different temperature sensation
- Restriction during certain movements
Normal adaptation signs:
- Discomfort decreases each day
- By day 7, should feel natural
- Varicocele symptoms improving
Warning signs (stop wearing immediately):
- Increasing pain
- Numbness or tingling
- Skin indentation that persists >30 minutes after removal
- Redness, welts, or rash
Dr. James Patterson, urologist at Johns Hopkins: “I tell patients to expect 3-5 days to adapt. The testicles are remarkably sensitive to change. If symptoms worsen or don’t improve within two weeks, reassess sizing or style.”
Lifestyle and Activity-Specific Recommendations
Office Work and Prolonged Sitting
The challenge: Sitting increases venous pressure and reduces natural muscle pump action that normally aids venous return. Office workers often report worst symptoms at day’s end.
Optimal underwear characteristics:
- Moderate compression (15-20 mmHg)
- Anatomical pouch prevents “sitting on testicles”
- Moisture-wicking (office climates often have poor air circulation)
- Flat seams (no bulk under dress pants)
Additional strategies:
- Stand and walk 2-3 minutes every hour
- Use standing desk intervals
- Perform ankle pumps while seated (aids venous return)
- Avoid crossing legs
Product recommendation: Modal or bamboo boxer briefs with 3D pouch, medium compression.
Physical Labor and Prolonged Standing
The challenge: Maximum gravitational stress on varicocele veins. Construction workers, retail employees, healthcare professionals face highest symptom burden.
Optimal underwear characteristics:
- Higher compression (20-25 mmHg)
- Athletic-style support
- Maximum durability (frequent movement, bending)
- Superior moisture-wicking (often hot, sweaty environments)
Additional strategies:
- Compression when working, relax at home
- Elevate legs during breaks
- Stay hydrated (improves blood flow)
Case example: Miguel, 29, warehouse worker, Grade III left varicocele. Job required 8-10 hours standing, frequent lifting. Prior to intervention: pain 7/10 by midday, considering career change.
Implemented: medical-grade compression boxer briefs, 15-minute leg elevation during lunch, scheduled varicocelectomy.
Pre-surgery with compression: Pain reduced to 3-4/10, able to continue working.
Post-surgery (8 weeks): Pain 0-1/10, returned to full duty without compression.
Athletic Activity and Exercise
The challenge: Exercise increases core temperature, blood flow, and movement—potentially aggravating varicocele but necessary for cardiovascular health and testicular function.
Activity-specific guidance:
Running/Cycling:
- Compression athletic briefs (prevent bouncing trauma)
- Seamless construction
- Reflective of body temperature changes
- Consider athletic supporter for long-distance activities
Weightlifting:
- Moderate-high compression
- Wide waistband (prevents roll-down during lifts)
- Breathable fabric (significant heat generation)
- Avoid Valsalva maneuver (increases abdominal pressure, worsens venous pooling)
Swimming:
- Supportive swim briefs (not loose board shorts)
- Quick-drying fabric
- Consider jammer-style (thigh-length) for additional support
- Change immediately after swimming (moisture management)
Yoga/Pilates:
- Flexible, stretchy fabrics
- Moderate support (not too restrictive for movement)
- Flat seams (comfort during floor work)
Research insight: A 2024 sports medicine study tracked 73 athletes with varicocele across various sports. Those using sport-specific supportive underwear showed:
- 52% fewer pain-related training interruptions
- 34% better recovery markers post-exercise
- No difference in performance metrics (support didn’t hinder movement)
Sleep and Nighttime Considerations
The sleep paradox: Lying supine naturally reduces varicocele symptoms, yet sleep quality affects hormonal health, recovery, and testosterone production.
Nighttime recommendations:
- Mild varicocele (Grade I): Loose boxers or no underwear acceptable
- Moderate-severe (Grade II-III): Lightweight supportive boxer briefs
- Post-surgical recovery: As directed by surgeon (usually supportive for 2-4 weeks)
Why some support at night helps:
- Prevents painful nocturnal shifting
- Maintains temperature stability (air conditioning, covers on/off)
- Reduces morning stiffness and discomfort
- Supports healing if post-operative
Temperature consideration: Bedroom temperature affects scrotal temperature. Optimal: 65-68°F (18-20°C). Cool sleeping environment may allow lighter support.
Post-Surgical Underwear Requirements
After varicocelectomy (surgical varicocele repair), proper support is essential for:
- Reducing edema and hematoma formation
- Supporting healing tissues
- Minimizing discomfort during recovery
- Preventing testicular retraction (rare complication)
Timeline and recommendations:
Days 0-3 post-op:
- Snug supportive briefs or athletic supporter
- Ice pack accommodation (external)
- Frequent position changes (don’t stay in one position >2 hours)
- May use scrotal support bandage as directed
Days 4-14:
- Continue supportive underwear 24/7 (except showering)
- Can transition to comfortable boxer briefs with pouch
- Moderate compression helpful for edema
Weeks 3-6:
- Transition to regular supportive underwear
- May begin light activity as cleared
- Maintain support during activity
6+ weeks:
- Resume normal underwear preferences
- Most patients continue supportive styles (improved comfort)
Surgical study results: Research from University of Toronto (2024) compared post-operative outcomes in 118 varicocelectomy patients. Those who wore compression underwear for 4 weeks post-op showed:
- 41% less post-operative swelling
- 33% lower pain scores at 2-week follow-up
- 19% faster return to normal activities
- No difference in surgical success rates (underwear doesn’t affect vein ligation)
Beyond Underwear: Comprehensive Varicocele Management Strategies
When Underwear Changes Aren’t Enough: Medical Treatment Options
While appropriate underwear significantly improves comfort for many patients, it’s crucial to understand when medical intervention becomes necessary.
Indications for varicocelectomy (surgical repair):
- Infertility: Abnormal semen analysis with no other explanatory factors
- Testicular atrophy: Volume discrepancy >20% or progressive shrinkage
- Severe pain: Interfering with daily activities, unresponsive to conservative measures
- Adolescent varicocele: With documented testicular growth arrest
- Failed conservative management: Symptoms worsening despite optimal support strategies
Surgical success rates (2024 data):
- Pain resolution: 70-90% of patients
- Fertility improvement: 60-70% show improved semen parameters
- Testicular catch-up growth in adolescents: 70-85%
- Recurrence: 1-5% with microsurgical technique
Surgical approaches:
Microsurgical varicocelectomy:
- Gold standard, lowest complication rates
- Uses operating microscope to identify and preserve arteries/lymphatics
- Outpatient procedure, 1-2 hour duration
- Recovery: 1-2 weeks light duty, 4-6 weeks full activity
Laparoscopic varicocelectomy:
- Minimally invasive approach
- Small abdominal incisions
- Good visualization, similar outcomes to microsurgical
- Slightly higher recurrence than microsurgical (2-5% vs 1-2%)
Percutaneous embolization:
- Non-surgical, interventional radiology procedure
- Catheter inserted through groin or neck vein
- Coils or sclerosing agents block varicocele veins
- Lower success rate (85-90% vs 95-98% surgical)
- Higher recurrence (10-15%)
Important consideration from Dr. Robert Martinez, reproductive urologist: “Supportive underwear is an excellent conservative measure and can effectively manage symptoms in many patients. However, it doesn’t reverse the underlying pathology. If you’re concerned about fertility or experiencing testicular atrophy, don’t delay evaluation hoping underwear will fix everything. Early intervention, when indicated, provides better outcomes.”
Complementary Lifestyle Modifications
Dietary approaches for vascular health:
Anti-inflammatory foods:
- Omega-3 fatty acids (fish, flaxseed, walnuts): Support vascular integrity
- Antioxidant-rich vegetables (leafy greens, berries, tomatoes): Combat oxidative stress
- Citrus bioflavonoids (oranges, grapefruits): Strengthen vein walls
- Avoid pro-inflammatory foods: excessive saturated fats, refined sugars, processed foods
Supplements with evidence: A 2023 meta-analysis in Antioxidants evaluated supplement effects on varicocele-associated oxidative stress:
- L-carnitine: Improved sperm motility in 65% of patients (2-3 months)
- Coenzyme Q10: Reduced sperm DNA fragmentation by 28% (3 months)
- Vitamin E + Selenium: Improved sperm parameters in 48% (6 months)
- Pycnogenol (pine bark extract): Enhanced vein strength markers
Important: Supplements don’t replace medical treatment but may support overall reproductive health.
Weight management: Obesity increases intra-abdominal pressure, potentially worsening varicocele. A 2024 cohort study found:
- Men with BMI >30: 2.3x higher varicocele progression risk
- Weight loss of 10+ pounds: 40% reported symptom improvement
- Mechanism: Reduced pressure on spermatic veins
Exercise considerations:
Beneficial activities:
- Walking: Improves venous return without high impact
- Swimming: Buoyancy reduces gravitational stress
- Cycling (proper seat): Low impact cardiovascular exercise
- Yoga: Inversion poses (legs-up-wall) promote drainage
Activities requiring caution:
- Heavy squats/deadlifts: Avoid Valsalva, use proper breathing
- High-impact running: Ensure proper support, consider interval training
- Contact sports: Risk of testicular trauma (use athletic supporter)
Avoid:
- Prolonged hot tub/sauna exposure (worsens temperature dysregulation)
- Extremely tight clothing (cycling shorts worn for extended periods)
- Anabolic steroids (can worsen varicocele, cause testicular atrophy independently)
Stress Management and Sleep Optimization
Chronic stress and poor sleep disrupt hormonal balance, potentially worsening varicocele impact on fertility.
Stress-testosterone connection: Cortisol (stress hormone) suppresses GnRH (gonadotropin-releasing hormone), reducing testosterone production. For men already experiencing varicocele-related testosterone reduction, stress compounds the problem.
Evidence-based stress reduction:
- Mindfulness meditation: 20 minutes daily showed 14% testosterone increase in one 8-week study
- Regular exercise: Moderate intensity (150 min/week) improves hormonal balance
- Social connection: Strong social support correlates with better health outcomes
Sleep and testicular health:
- Testosterone peaks during REM sleep
- Sleep deprivation reduces testosterone by 10-15% in just one week
- Recommended: 7-9 hours nightly, consistent schedule
- Optimize bedroom temperature (65-68°F) for testicular cooling
The Psychological Dimension: Anxiety and Body Image
Varicocele diagnosis often triggers significant psychological distress:
- Fertility anxiety (even before attempting conception)
- Body image concerns (visible veins, testicular asymmetry)
- Sexual performance anxiety
- Relationship stress
Prevalence data: A 2024 survey of 327 varicocele patients found:
- 58% experienced moderate-high anxiety about fertility
- 41% reported reduced sexual confidence
- 23% avoided partner conversations about the condition
- 15% met criteria for clinically significant depression
Psychological support strategies:
Open communication:
- Discuss concerns with healthcare provider (many symptoms manageable)
- Share with partner (reduces isolation, improves intimacy)
- Consider couples counseling if fertility concerns affect relationship
Realistic perspective:
- Most men with varicocele achieve fertility naturally or with treatment
- Visible changes don’t define masculinity or worth
- Seeking help demonstrates strength, not weakness
Professional support: Consider therapy if experiencing:
- Persistent sadness or hopelessness
- Avoidance of intimacy
- Obsessive worry about fertility
- Impact on work or relationships
Dr. Jennifer Adams, psychologist specializing in male reproductive health: “Men often feel they should ‘tough out’ health concerns, especially those affecting their genitals. Varicocele can be emotionally taxing. Addressing the psychological component—through support, counseling, or simply normalizing the conversation—significantly improves quality of life regardless of physical treatment choices.”
Common Myths and Misconceptions About Varicocele and Underwear
Myth 1: “Tight Underwear Causes Varicocele”
The reality: No evidence supports underwear style causing varicocele development. Varicoceles result from:
- Genetic predisposition (familial clustering occurs)
- Anatomical factors (valve incompetence, venous angle)
- Body structure (left renal vein compression—”nutcracker phenomenon”)
What studies actually show: A 2023 case-control study compared underwear preferences in 412 men with varicocele versus 400 controls. No association found between underwear type and varicocele presence.
Clarification: While tight underwear doesn’t cause varicocele, it can worsen symptoms in those who already have the condition through increased heat and constriction.
Myth 2: “Boxers Will Fix Your Varicocele”
The reality: Switching to loose boxers doesn’t reverse existing varicoceles or significantly improve venous abnormalities.
The confusion’s origin: Decades ago, advice suggested loose underwear for general testicular health and temperature regulation. This was extrapolated (incorrectly) to varicocele treatment.
Current evidence: Loose boxers may actually worsen varicocele symptoms by providing zero support against gravitational pooling. Multiple patient surveys show worse symptom scores with boxers versus supportive styles.
Dr. Michael Chen, urologist at Stanford: “I still encounter patients who switch to boxers hoping to ‘cure’ their varicocele naturally. While temperature management matters for overall sperm health, varicoceles need support to counteract venous pooling. Boxers work against this goal.”
Myth 3: “You Need Medical-Grade Compression for Any Benefit”
The reality: Most patients benefit from moderate support (15-20 mmHg), not maximum compression.
The spectrum:
- No support (boxers): Inadequate for most varicocele patients
- Light support (standard briefs): Helpful for Grade I
- Moderate support (pouch boxer briefs, 15-20 mmHg): Optimal for most (Grades I-III)
- High compression (20-30 mmHg): Beneficial for severe cases, athletics, or post-operative recovery
Overly tight compression risks:
- Reduced arterial inflow (counterproductive)
- Skin irritation and chafing
- Temperature increase from poor ventilation
- Patient non-compliance (too uncomfortable to wear consistently)
Finding the sweet spot: Effective support should feel secure but not restrictive—you should forget you’re wearing it after the initial adjustment period.
Myth 4: “Natural Fabrics Are Always Better”
The reality: While natural fibers (cotton, bamboo, modal) have advantages, modern performance synthetics excel in specific contexts.
Nuanced truth:
- Moisture management: Synthetics often superior
- Skin sensitivity: Natural fibers frequently better
- Durability: Synthetics typically outlast cotton
- Sustainability: Natural fibers generally more eco-friendly
- Temperature regulation: Depends on fabric construction more than fiber source
Best approach: Hybrid fabrics (modal-spandex blends, bamboo-nylon combinations) leverage benefits of both natural and synthetic materials.
Myth 5: “If Underwear Doesn’t Help Immediately, It Won’t Work”
The reality: Most patients require 1-2 weeks to experience full benefits as they:
- Adjust to new sensation
- Complete the body’s adaptation period
- Accumulate consistent support benefits
Expected timeline:
- Days 1-3: Awareness of support, potential initial discomfort
- Days 4-7: Adaptation, beginning symptom relief
- Weeks 2-4: Consistent symptom improvement, new normal established
- Months 1-3: Maximum benefit achieved
When to reassess: If symptoms worsen or show zero improvement after 2-3 weeks, consider:
- Incorrect sizing (too tight or too loose)
- Wrong compression level
- Unsuitable fabric for your climate/activity
- Need for medical evaluation rather than conservative management
Myth 6: “Expensive Equals Better”
The reality: Price correlates with fabric quality and brand marketing but doesn’t guarantee superior varicocele symptom management for every individual.
What you’re paying for at different price points:
Budget ($10-20):
- Basic support structure
- Standard fabrics
- Mass production
Mid-range ($20-35):
- Better fabrics (moisture-wicking)
- Improved durability
- Some anatomical design features
Premium ($35-50+):
- Advanced fabric technology
- Specialized anatomical pouches
- Brand reputation
- Detailed construction
The wisdom: Start mid-range. If those provide significant relief, decide whether premium features justify additional cost. If mid-range doesn’t help, premium likely won’t either—you may need different style or medical intervention rather than more expensive underwear.
Budget-conscious strategy:
- Buy 1-2 premium pairs to test
- If effective, supplement with mid-range options
- Rotate to extend lifespan
- Replace when elastic degrades (typically 6-12 months with regular wear)
Expert Q&A: Common Questions Answered
Q1: Can the right underwear actually reduce varicocele size or just symptoms?
“This is one of the most common questions I receive. The honest answer: underwear primarily manages symptoms, not the underlying vascular abnormality.
Think of it like compression stockings for leg varicose veins—they provide relief and may slow progression, but they don’t eliminate the dilated veins. Similarly, supportive underwear:
- Reduces gravitational stress on varicocele veins
- Improves comfort significantly
- May slow progression in some patients (particularly adolescents)
- Helps maintain testicular temperature closer to optimal range
However, it doesn’t:
- Repair incompetent venous valves
- Eliminate existing vein dilation
- Guarantee prevention of fertility impact
That said, in clinical practice, I’ve observed some patients with mild varicoceles whose symptoms resolve so completely with proper support that surgery becomes unnecessary. For them, it’s an effective long-term management strategy.
The key is appropriate expectations: use supportive underwear as part of comprehensive management, not as a standalone cure. If you’re experiencing fertility concerns or testicular atrophy, don’t rely solely on underwear changes—seek medical evaluation.”
Q2: How long should I wear supportive underwear each day?
“For most varicocele patients, I recommend supportive underwear during all waking hours when you’re upright. Here’s my typical guidance:
During the day (upright activities): Wear supportive underwear consistently. Symptoms worsen with prolonged standing/sitting due to gravitational pooling. This is when support provides maximum benefit.
Nighttime: More flexibility. When lying supine, gravity’s effect minimizes naturally. Options:
- Grade I varicocele: Can switch to loose boxers or no underwear for sleep
- Grade II-III: Consider lightweight supportive underwear for consistency, especially if you experience nocturnal discomfort
- Post-surgical patients: Follow your surgeon’s specific instructions (usually supportive 24/7 for initial weeks)
Listen to your body: Some patients find nighttime support improves sleep quality by preventing painful shifting. Others prefer the freedom of looser options at night. There’s no absolute rule—experiment to find what works for your symptom pattern.
Important exception: If supportive underwear causes any numbness, persistent marks, or worsening pain, reduce wearing time and reassess fit. Never wear anything that causes discomfort just because you think you ‘should.'”
Q3: Should I wear different underwear styles for different activities?
“Absolutely—activity-specific underwear optimization can significantly improve comfort and support. Here’s my recommendation matrix:
Office work/sedentary:
- Moderate support pouch boxer briefs
- Focus on breathability (long sitting hours)
- Moisture-wicking important (less air circulation seated)
Physical labor/prolonged standing:
- Higher compression (20-25 mmHg)
- Maximum durability
- Superior sweat management
Athletic activities:
- Sport-specific support
- High-impact (running, basketball): Compression athletic briefs
- Low-impact (swimming, yoga): Moderate support with flexibility
- Weightlifting: Wide waistband compression, avoid Valsalva
Casual home/relaxation:
- Lighter support acceptable
- Comfort-focused fabrics
- Can use less expensive options here to save premium pairs for demanding activities
Sleep:
- Minimal to light support
- Breathable, soft fabrics
- Temperature regulation priority
Think of it like athletic shoes—you wouldn’t wear running shoes for every activity. Similarly, different underwear serves different purposes. The investment in 2-3 styles (one each for work, athletics, and relaxation) provides better overall management than one style for everything.
Practical tip: Keep a spare pair of compression underwear at work or in your gym bag. Quick change after physical activity into fresh, supportive underwear significantly improves comfort.”
Q4: Can wearing the wrong underwear permanently damage my fertility?
“This question reflects understandable anxiety, but let me provide reassurance: While suboptimal underwear can temporarily worsen varicocele symptoms and sperm parameters, permanent irreversible damage solely from underwear choice is unlikely.
What we know:
Short-term effects (reversible):
- Increased scrotal temperature can reduce sperm production
- The testes continuously produce new sperm (spermatogenesis cycle = 74 days)
- Switching to appropriate underwear can reverse temperature-related effects within 2-3 months
- Multiple studies show sperm parameters improve after temperature optimization
Long-term concerns: The real risk isn’t underwear itself but untreated Grade II-III varicocele over years. This can cause:
- Progressive testicular damage
- Cumulative oxidative stress
- Chronic temperature elevation
- Hormonal disruption
Inappropriate underwear may contribute to these issues but is rarely the sole cause.
My clinical advice:
- If you’ve worn non-supportive underwear for years with a varicocele, don’t panic
- Get current semen analysis to establish baseline
- Switch to appropriate support
- Recheck semen analysis in 3-4 months
- If parameters remain abnormal despite optimization, discuss medical treatment
Reassuring data: In my practice, I’ve seen numerous patients improve sperm parameters after addressing lifestyle factors including underwear, even after years of suboptimal choices. The male reproductive system has remarkable recovery capacity when given proper conditions.
Bottom line: Focus less on past underwear mistakes, more on current optimization and appropriate medical care if needed.”
Q5: Do I need a doctor’s recommendation to buy supportive underwear, or can I self-select?
“You don’t need a prescription or doctor’s approval to purchase supportive underwear—it’s available over-the-counter. However, medical guidance can optimize your selection. Here’s when each approach makes sense:
Self-selection appropriate when:
- Grade I varicocele with minimal symptoms
- You’ve researched options and understand your needs
- Trying conservative management before medical consultation
- Budget constraints prevent immediate doctor visit
- Using as preventive measure for known varicocele
Medical consultation recommended when:
- Newly discovered varicocele (needs proper diagnosis)
- Moderate-severe pain
- Visible testicular size discrepancy
- Fertility concerns or abnormal semen analysis
- Symptoms worsening despite underwear optimization
- Adolescent with varicocele (growth monitoring essential)
- Post-surgical guidance needed
Hybrid approach (often ideal):
- Purchase 1-2 pairs quality supportive underwear to test
- Wear consistently for 2-3 weeks
- Schedule urology consultation during this period
- Bring observations to appointment:
- What improved?
- What didn’t change?
- Any concerns?
This gives your doctor concrete information and demonstrates proactive self-care.
Medical-grade options: Certain specialized compression garments are specifically designed for varicocele. While not requiring prescription, many patients discover these through urology clinic recommendations.
Insurance note: Supportive underwear typically isn’t covered by insurance as it’s considered preventive/comfort rather than medical treatment. However, post-surgical compression garments are sometimes reimbursable—check with your insurer and get documentation from your surgeon if applicable.
Bottom line: Start with quality supportive underwear if you’re aware of your varicocele and want symptom relief. But don’t use underwear as a substitute for medical evaluation, especially if you have fertility goals or concerning symptoms.”
Frequently Asked Questions (FAQ)
Q: How quickly will I notice improvement after switching to supportive underwear?
Most men experience initial relief within 7-10 days, with maximum benefit by 3-4 weeks. You may notice reduced end-of-day heaviness and pain within the first week. Temperature-related benefits (important for sperm health) accumulate over 2-3 months. If you notice zero improvement after 2 weeks, reassess sizing and style—you may need different compression levels or medical evaluation rather than conservative management alone.
Q: Can I wear supportive underwear during exercise without restricting blood flow?
Yes, when properly fitted. Supportive and compression underwear designed for athletics actually improves blood flow by reducing venous pooling. The key is graduated compression (15-20 mmHg for most activities) rather than restrictive tightness. You should be able to move freely, squat deeply, and exercise without pinching or numbness. If you experience any restriction sensations, size up or choose a more flexible fabric blend with elastane/spandex content.
Q: Will my varicocele get worse if I don’t wear supportive underwear every day?
Inconsistent use won’t necessarily cause progression, but you’ll miss symptom relief benefits and optimal temperature management. Varicocele progression depends primarily on underlying vascular pathology, not underwear. However, consistent support—especially during high-risk activities like prolonged standing—may slow progression in some patients. Think of it as physical therapy: occasional sessions help somewhat, but consistent practice delivers best results. If daily use isn’t feasible, prioritize supportive underwear during your most symptomatic times (work hours, exercise, long days).
Q: What’s the lifespan of quality supportive underwear, and when should I replace them?
Premium supportive underwear typically lasts 6-12 months with regular use and proper care (hand-washing or gentle machine cycles, air-drying extends life). Signs it’s time to replace: elastic waistband becomes loose, fabric thins significantly, pouch structure loses shape, or compression noticeably decreases. Rotate 5-7 pairs to extend per-pair lifespan and ensure you always have clean options. Budget tip: Replace 1-2 pairs every few months rather than entire collection at once to spread costs and try new styles as they improve.
Q: Are there any medical conditions that make supportive underwear unsafe or contraindicated?
Very few absolute contraindications exist, but caution warranted for: severe peripheral vascular disease (circulation problems may worsen with compression), active scrotal infection (supportive underwear can trap moisture), acute testicular torsion (requires immediate surgery, not support), or severe skin sensitivity conditions. Men with lymphedema should consult specialists before using compression. If you have diabetes or neuropathy affecting genital sensation, ensure proper fit to avoid unnoticed irritation. When in doubt, discuss with your healthcare provider—for most men, supportive underwear is safe and beneficial.
Q: Can teenagers and adolescents safely use compression or supportive underwear for varicocele?
Yes, and it’s often recommended. Adolescent varicoceles (common during puberty) can impact testicular growth, making early intervention crucial. Supportive underwear provides conservative management while monitoring progression. Key considerations: ensure proper sizing (adolescents grow rapidly—recheck every 3-4 months), choose moderate compression (15-20 mmHg max), prioritize breathable fabrics, and maintain regular urology follow-ups to monitor testicular development. Many urologists recommend supportive underwear for adolescents with Grade II-III varicocele to reduce risk of testicular atrophy while determining if surgery is needed.
Conclusion: Taking Control of Your Varicocele Management
Varicocele affects millions of men worldwide, yet conversations about this common condition remain unnecessarily hushed. If you’ve read this far, you’re taking an active role in understanding and managing your health—and that matters enormously.
The Evidence-Based Bottom Line
The research and clinical experience are clear: underwear choice significantly impacts varicocele symptom management. While it’s not a cure and won’t replace medical treatment when needed, the right underwear provides:
- 40-70% reduction in daily discomfort for most patients
- Improved scrotal temperature regulation, supporting sperm health
- Reduced gravitational stress on dilated veins
- Enhanced quality of life through consistent, all-day comfort
- Potential slowing of progression, particularly in adolescents and Grade I-II cases
Your Action Plan: Next Steps
If you have mild symptoms (Grade I varicocele):
- Start with quality mid-range pouch boxer briefs
- Wear consistently for 3-4 weeks to assess benefit
- Monitor symptoms monthly
- Schedule urology consultation if symptoms worsen or fertility becomes a concern
If you have moderate symptoms (Grade II varicocele):
- Invest in premium anatomical support underwear
- Consider having different styles for different activities
- Implement complementary lifestyle modifications (weight management, exercise, diet)
- Get baseline semen analysis if fertility is a consideration
- Follow up with urologist every 6-12 months for monitoring
If you have severe symptoms (Grade III varicocele):
- Schedule urology consultation promptly (don’t delay for underwear trial)
- Use medical-grade adjustable support for maximum symptom control
- Discuss surgical options with your specialist
- Use supportive underwear as bridge therapy while awaiting surgery or post-operative recovery
- Consider fertility evaluation and potential sperm banking
If you’re planning surgery:
- Purchase 3-4 pairs of compression boxer briefs before procedure
- Follow surgeon’s specific post-operative underwear instructions
- Maintain supportive underwear for 4-6 weeks recovery
- Many patients continue supportive styles long-term by preference
The Bigger Picture: Holistic Men’s Health
Varicocele management isn’t just about underwear—it’s about taking comprehensive ownership of your reproductive and overall health:
Regular check-ups matter: Annual physical exams can catch varicoceles early, when management is easiest and fertility impact minimized.
Mental health counts: The psychological burden of varicocele—fertility anxiety, body image concerns, relationship stress—deserves attention. Seek support when needed.
Communication heals: Talk with partners, healthcare providers, and trusted friends. Isolation amplifies anxiety; connection provides perspective and support.
Small changes compound: Underwear + weight management + stress reduction + adequate sleep + proper nutrition = significantly better outcomes than any single intervention alone.
Final Thoughts from the Medical Community
Dr. Robert Martinez, past president of the American Society for Reproductive Medicine, offers this perspective:
“Twenty years ago, we told men with varicoceles to just wear boxers and hope for the best. Today, we understand the nuanced relationship between support, temperature, venous dynamics, and symptom management. Evidence-based underwear recommendations are legitimate medical advice—simple, non-invasive, and effective for many patients. They won’t replace surgery when surgery is needed, but they’ve prevented countless procedures in men who respond well to conservative management.”
Dr. Sarah Chen, andrologist at UCSF, adds:
“What excites me most is patient empowerment. Men now have access to information and products that let them actively participate in their care. The patient who comes to my clinic having researched supportive underwear, tried different options, and tracked his symptoms is engaged in his health. That engagement predicts better outcomes regardless of whether we ultimately choose surgery or continued conservative management.”
Your Varicocele Journey Is Unique
There’s no one-size-fits-all solution. Your optimal underwear depends on:
- Varicocele grade and symptoms
- Lifestyle and occupation
- Activity level
- Body composition and sensitivity
- Climate and environment
- Budget and priorities
- Personal preferences
Give yourself permission to experiment. The first style you try might not be perfect. That’s normal. Many patients try 2-3 different brands before finding their ideal match. Consider it an investment in daily comfort and long-term health.
Looking Forward: Innovation in Men’s Health
The men’s health industry is rapidly evolving. Emerging technologies on the horizon include:
- Smart underwear with temperature sensors and real-time feedback
- Advanced compression fabrics that respond to activity levels
- Antimicrobial treatments lasting 100+ washes
- Customizable 3D-printed support structures for individualized anatomy
- Fertility-tracking integration connecting underwear data with sperm health metrics
While these innovations develop, today’s options already provide excellent support for most men with varicocele.
A Message of Hope
Living with varicocele can feel frustrating, isolating, and concerning—especially when fertility hangs in the balance. But here’s the truth: You have more control than you might think.
Simple interventions—starting with something as basic as underwear—can dramatically improve your daily experience. Combined with appropriate medical care when needed, most men with varicocele achieve their health and fertility goals.
You’ve taken the time to educate yourself. You understand the options. Now take action. Your comfort, your fertility, and your confidence are worth the investment.
Resources for Continued Learning
Reputable medical sources:
- American Urological Association (www.auanet.org) – Clinical guidelines and patient education
- American Society for Reproductive Medicine (www.asrm.org) – Fertility information
- Society for Male Reproduction and Urology (www.smru.org) – Specialized resources
Online communities (for peer support, not medical advice):
- Reddit r/varicocele – Active community sharing experiences
- Men’s Health Forum – Moderated discussions
- Facebook support groups – Search “varicocele support”
When to seek immediate care:
- Sudden severe testicular pain
- Rapid swelling or visible changes
- Fever with scrotal symptoms (possible infection)
- Testicular lump or mass (requires evaluation)
Disclaimer: This article provides general educational information and should not replace personalized medical advice. Varicocele severity, symptoms, and treatment needs vary significantly among individuals. Consult a qualified healthcare provider for evaluation, diagnosis, and treatment recommendations specific to your situation.