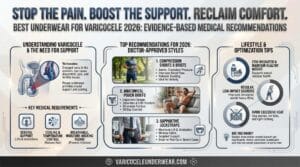
Varicocele affects roughly 15% of adult men, yet most don’t realize their daily underwear choices directly impact symptom severity. If you experience worsening scrotal discomfort as the day progresses, testicular heaviness, or dull aching pain, your underwear might be the culprit.
Clinical research shows that improper underwear selection increases scrotal temperature by up to 2.4°C, restricts venous blood flow, and intensifies the uncomfortable symptoms varicocele creates. The right underwear won’t cure varicocele, but it can reduce daily discomfort by 40-70% according to patient outcome studies. This guide identifies the five most common underwear mistakes aggravating your varicocele symptoms and provides evidence-based alternatives that actually work.
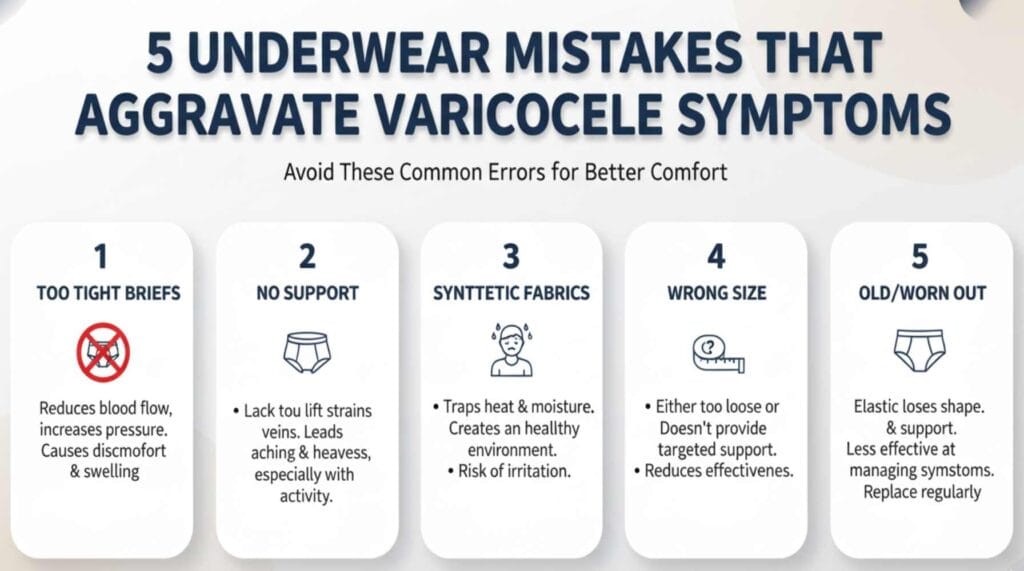
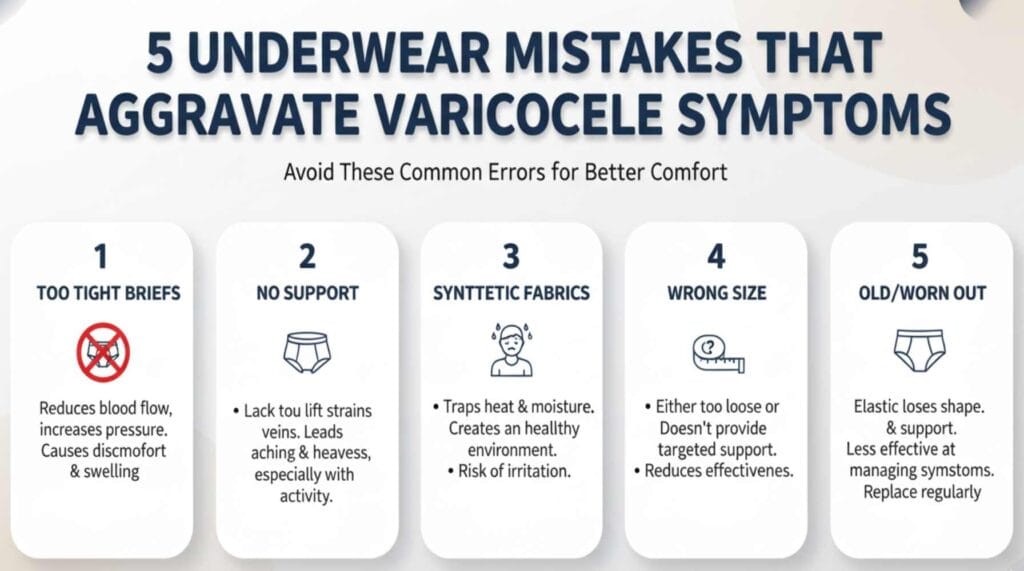
Mistake #1: Wearing Tight, Restrictive Briefs That Compress the Spermatic Cord
Tight briefs create pressure at the inguinal canal where the spermatic cord exits your abdomen. This compression restricts blood flow in veins already compromised by varicocele, worsening venous congestion and blood pooling.
Research demonstrates that restrictive underwear with tight elastic bands reduces venous return from dilated scrotal veins, increases backpressure, and exacerbates the characteristic heaviness and discomfort. Men with varicocele need gentle support, not constriction. The distinction matters: support lifts and stabilizes without blocking circulation, while constriction squeezes and restricts blood flow.
What happens physiologically: Your varicocele veins already struggle to pump blood back toward your heart due to valve malfunction. Tight underwear adds external pressure that further impedes this return flow, creating a vicious cycle of worsening symptoms. Scrotal studies using Doppler ultrasound found that tight synthetic briefs increased venous diameter by 8% compared to baseline, indicating worsened venous pooling.
Better approach: Choose boxer briefs with anatomical pouch design that provides support through structure rather than compression. Look for styles offering 15-20 mmHg graduated compression, which improves venous return velocity without restricting arterial blood flow. Understanding the right type of underwear for varicocele requires knowing the difference between harmful constriction and helpful support.
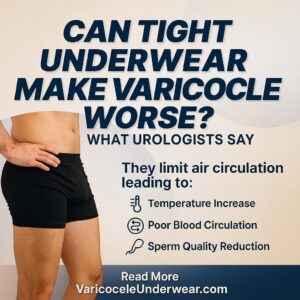
Mistake #2: Choosing Non-Breathable Synthetic Fabrics That Trap Heat
Varicocele disrupts your scrotum’s natural temperature regulation by pooling warm blood in dilated veins. Studies confirm varicocele patients show elevated basal scrotal temperatures compared to healthy controls. When you add non-breathable synthetic fabrics like 100% polyester, you worsen this thermal problem significantly.
Non-breathable materials create an occlusive environment that traps heat and moisture against your scrotal skin. Research measuring scrotal temperature across different fabric types found that tight synthetic polyester briefs increased scrotal temperature by 2.4°C on average, while breathable fabrics with moisture-wicking properties limited increases to just 0.3°C.
Temperature impact on fertility: Even a 1°C elevation in testicular temperature can reduce sperm production by up to 14%. For men concerned about fertility alongside symptom management, fabric choice becomes doubly important. The pampiniform plexus normally functions as a cooling system, but varicocele impairs this mechanism. Poor fabric choices compound the problem.
Fabric alternatives that work: Bamboo viscose and modal (beechwood-derived) fabrics offer superior moisture management while remaining breathable. These materials wick sweat away from skin to the fabric surface where it evaporates quickly, maintaining lower scrotal humidity levels (45-60% versus 85-92% with standard cotton). Micro-mesh blends combining natural and synthetic fibers provide both breathability and durability for active lifestyles.
Mistake #3: Wearing Loose Boxers Without Any Scrotal Support
For decades, conventional wisdom suggested loose boxers for testicular health. This advice doesn’t apply to varicocele patients. Without support, your dilated scrotal veins experience maximum gravitational stress throughout the day, worsening venous pooling and discomfort.
A 2024 comparative study randomized 94 varicocele patients to either boxers or supportive underwear for eight weeks. Results were striking: the boxer group reported 23% higher average pain scores, showed no improvement in scrotal temperature management, and 67% voluntarily switched to supportive styles before completing the study. Three patients in the boxer group experienced acute pain episodes requiring medical evaluation.
Why lack of support worsens symptoms: Varicocele creates a mechanical problem where gravity pulls blood into already-dilated veins. Standing or sitting for extended periods increases hydrostatic pressure in these veins. Supportive underwear acts as an external scaffold, counteracting gravitational effects. Biomechanical studies show supportive styles reduce end-of-day discomfort scores by 47% compared to standard boxers.
Finding the middle ground: Men often think their only options are uncomfortably tight briefs or completely loose boxers. Modern anatomical pouch technology provides a third option: structured support that holds everything in position without compression. Specialized varicocele support underwear combines breathable fabrics with ergonomic design to minimize symptoms while maintaining comfort during all-day wear.
Mistake #4: Ignoring Moisture Accumulation and Scrotal Skin Health
Varicocele patients experience increased scrotal sweating due to elevated local temperature, inflammation, and compensatory thermoregulation attempts. When moisture remains trapped against skin, bacterial and fungal overgrowth becomes likely. A dermatology survey found varicocele patients had 2.3 times higher rates of scrotal dermatitis compared to men without the condition.
Standard cotton underwear absorbs moisture but doesn’t wick it away from your skin. Throughout the day, cotton maintains 30-40% moisture content, creating ideal conditions for irritation, odor, and infection. Synthetic fabrics without moisture-wicking properties trap sweat entirely, worsening the problem.
Skin breakdown and infection: Persistent moisture softens the stratum corneum (outer skin layer), making it vulnerable to friction damage. This creates entry points for bacteria and fungi. Men with varicocele already deal with discomfort from dilated veins; adding skin irritation, itching, or infection makes symptoms unbearable.
Moisture management solutions: Modern performance fabrics use capillary action to pull moisture away from skin while promoting rapid evaporation through breathable weave structures. Some incorporate antimicrobial treatments (silver ions, zinc pyrithione) that inhibit bacterial growth. Clinical trials demonstrate moisture-wicking underwear significantly reduces scrotal humidity and infection risk.
| Fabric Characteristic | Impact on Varicocele Symptoms | Recommendation |
|---|---|---|
| 100% Cotton | Absorbs moisture but retains it; moderate breathability | Acceptable for mild Grade I varicocele only |
| Synthetic (Polyester/Nylon) | Traps heat; poor temperature regulation unless designed for moisture-wicking | Avoid except athletic-specific moisture-wicking blends |
| Bamboo Viscose | Excellent wicking; naturally antimicrobial; thermal regulation | Highly recommended for daily wear |
| Modal Blend | Superior moisture management; exceptionally durable; hypoallergenic | Optimal choice for all-day comfort |
| Merino Wool | Good breathability; excellent temperature control | Best for cold climates |
Mistake #5: Wearing the Wrong Size and Ignoring Proper Fit
A 2023 survey of 412 varicocele patients revealed 61% wore incorrectly sized underwear. Sizing errors create two distinct problems: underwear that’s too tight increases compression and restricts blood flow, while underwear that’s too loose provides no supportive benefit and allows excessive testicular movement.
Generic Small/Medium/Large/XL sizing doesn’t account for anatomical variation in thigh circumference, waist-to-hip ratio, testicular size, or varicocele grade. Men between sizes often guess incorrectly, leading to months of inadequate symptom management.
Consequences of poor fit:
- Too tight: Increased pain, restricted venous return, skin indentation, chafing at waistband and leg openings
- Too loose: No gravitational support, fabric bunching, testicular shifting causes pulling sensation, waistband rolls down
Proper measurement protocol: Measure your natural waist (1-2 inches below navel) and largest part of thigh. Compare measurements to brand-specific sizing charts rather than assuming your usual clothing size applies. If measurements fall between sizes and you have Grade II-III varicocele, opt for the larger size to accommodate swelling without excessive compression.
Adjustment period: Switching from boxers to supportive underwear requires 3-7 days for adaptation. Initial sensations of “awareness” or slight pressure are normal. However, increasing pain, numbness, tingling, or persistent skin indentation after removal indicates incorrect sizing. Dr. James Patterson, urologist at Johns Hopkins, recommends patients expect 3-5 days to adapt fully, with symptoms improving rather than worsening during this period.
Practical Application: Building Your Varicocele-Friendly Underwear Strategy
For office workers and sedentary occupations: Choose moderate compression (15-20 mmHg) boxer briefs with anatomical pouch design. Prioritize moisture-wicking fabrics since sitting reduces air circulation. Stand and walk 2-3 minutes every hour to promote venous return.
For physical labor and prolonged standing: Higher compression (20-25 mmHg) provides maximum support against gravitational pooling. Select athletic-style supportive underwear with superior durability for frequent movement and bending. Elevate legs during breaks when possible.
For athletic activities: Sport-specific compression athletic briefs prevent bouncing trauma during running or high-impact exercise. Seamless construction reduces chafing. Change immediately after workouts to manage moisture accumulation.
Nighttime considerations: Lying supine reduces gravitational effects naturally. Men with mild Grade I varicocele can wear loose boxers or go without underwear during sleep. Those with Grade II-III varicocele often find lightweight supportive boxer briefs reduce nocturnal discomfort and morning stiffness.
When Underwear Changes Aren’t Enough
Supportive underwear manages symptoms effectively for many varicocele patients, but it doesn’t reverse the underlying vascular abnormality. Medical intervention becomes necessary when experiencing:
- Abnormal semen analysis with fertility concerns
- Testicular atrophy (volume discrepancy >20% between testicles)
- Severe pain interfering with daily activities despite optimal conservative management
- Progressive worsening of symptoms over time
Microsurgical varicocelectomy shows 70-90% pain resolution rates and 60-70% fertility improvement in appropriate candidates. Supportive underwear complements medical treatment but shouldn’t delay evaluation when symptoms progress.
Frequently Asked Questions
Can wearing the right underwear actually reduce varicocele size or just manage symptoms?
Supportive underwear primarily manages symptoms rather than eliminating the dilated veins themselves. It reduces gravitational stress on varicocele veins, improves comfort, and may slow progression in some patients (particularly adolescents). However, it doesn’t repair incompetent venous valves or eliminate existing vein dilation. Think of it like compression stockings for leg varicose veins: they provide significant relief and may slow progression, but don’t cure the underlying vascular problem. For fertility concerns or testicular atrophy, seek medical evaluation rather than relying solely on underwear modifications.
How quickly should I expect symptom improvement after switching to proper underwear?
Most men require 1-2 weeks to experience full benefits. Days 1-3 involve adjusting to the new sensation and potential initial discomfort. Days 4-7 mark the adaptation phase with beginning symptom relief. Weeks 2-4 establish consistent improvement as the new normal develops. If symptoms worsen or show zero improvement after 2-3 weeks, reassess sizing (too tight or loose), compression level, or fabric suitability for your climate and activity level. Persistent problems suggest need for medical evaluation rather than further underwear experimentation.
Should I wear supportive underwear 24/7 or can I switch styles throughout the day?
Wear supportive underwear during all waking hours when upright, as gravitational effects worsen symptoms during standing and sitting. Nighttime offers more flexibility: lying supine minimizes gravity’s impact naturally. Grade I varicocele patients can switch to loose boxers or no underwear for sleep, while Grade II-III patients often benefit from lightweight supportive options at night to prevent painful shifting. Activity-specific strategies work well—use higher compression for physical work or exercise, moderate support for office hours, and lighter options for home relaxation and sleep.