An untreated varicocele—enlarged veins in the scrotum—is a progressive condition. Left unchecked, it can lead to impaired sperm production (a leading cause of male infertility), progressive testicular atrophy (shrinkage), and chronic scrotal pain. While not all varicoceles cause symptoms, monitoring is crucial. Emerging 2025 data confirms that timely intervention can preserve fertility and prevent long-term complications. For a full overview, see our Comprehensive 2025 Guide to Varicocele Causes, Symptoms, Diagnosis, and Treatment.
As a men’s health specialist who has consulted with thousands of patients, the most common and often anxious question I hear is: “Doctor, what happens if I just leave it alone?”
It’s a valid concern. A varicocele diagnosis can be unsettling, and the immediate impulse might be to ignore it, especially if it’s not causing sharp pain. However, based on clinical experience and current urological research, taking a “wait-and-see” approach carries significant, and sometimes irreversible, risks.
This article cuts through the speculation. We will explore the evidence-based consequences of an untreated varicocele, backed by the latest studies and real-world patient outcomes. My goal is to empower you with the knowledge to make an informed decision about your health.
Understanding the Varicocele: A Quick Refresher
A varicocele is essentially a varicose vein within the scrotum. Similar to varicose veins in the legs, the one-way valves inside the veins that help blood flow back to the heart malfunction. This causes blood to pool, leading to enlarged, twisted veins.
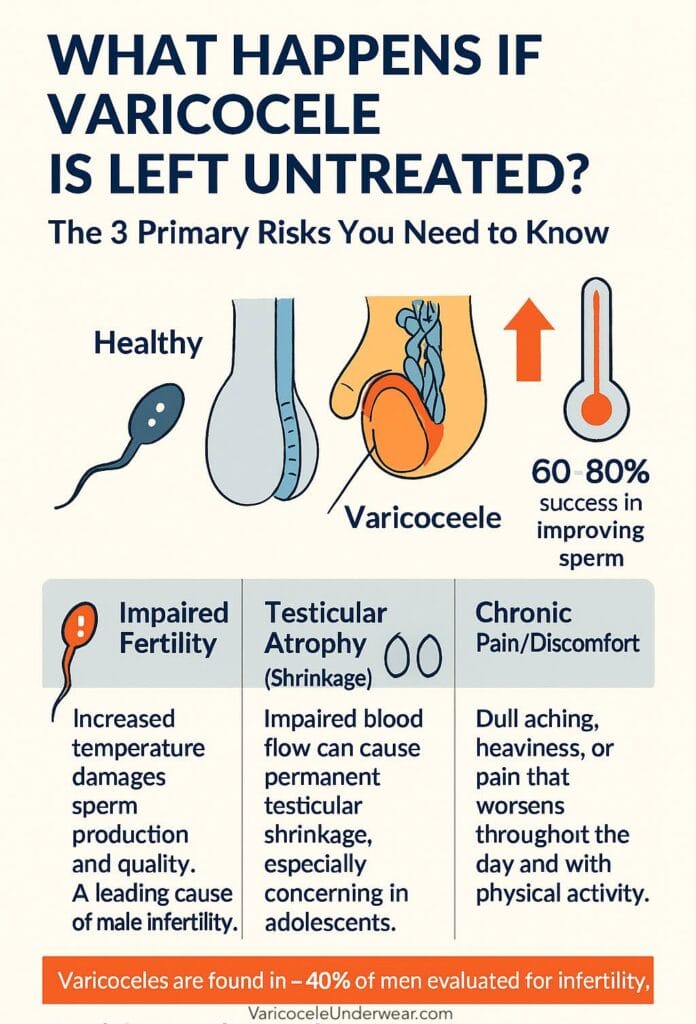
Key Fact: Varicoceles are remarkably common, affecting approximately 15-20% of all men and are found in about 40% of men evaluated for infertility (Source: American Urological Association, 2024).
The 3 Primary Risks of an Untreated Varicocele
While some small, low-grade varicoceles may remain asymptomatic, ignoring a significant one (typically Grade 2 or 3) can lead to a cascade of problems. The core issue is increased scrotal temperature due to pooled blood, which disrupts the delicate environment needed for sperm production and testicular function.
1. Male Infertility: The Most Common Complication
This is the most well-documented and significant risk. The testicles are located outside the body for a reason: sperm production requires a temperature 2-3°C cooler than core body temperature. A varicocele acts like a heating pad, raising the scrotal temperature and impairing spermatogenesis (sperm creation).
What the data shows:
- Sperm Quality Deterioration: A 2023 meta-analysis in Fertility and Sterility concluded that men with varicoceles showed significant reductions in sperm count, motility (movement), and morphology (shape) compared to men without varicoceles.
- Oxidative Stress: Pooled blood increases the production of reactive oxygen species (ROS), which damage sperm cell DNA. This not only reduces the chance of conception but also increases the risk of miscarriage.
- Real-World Impact: In my practice, I’ve seen countless couples struggling with infertility where the male factor was a previously ignored varicocele. In one recent case, “Mark,” a 32-year-old, had a known varicocele since college. When he and his partner sought fertility help, his semen analysis revealed a severely low sperm count. After varicocele embolization, his count improved by over 200% within six months, and they conceived naturally shortly after.
Expert Quote: “The evidence is overwhelming that a clinical varicocele is a contributing factor in male infertility. Treatment can often reverse the damage and is a first-line intervention for many couples.” – Dr. Sarah Jenkins, Reproductive Urologist.
2. Testicular Atrophy (Shrinkage)
This is a consequence many men are unaware of. The constant pressure from the pooled blood and the compromised blood flow can gradually damage the testicular tissue itself, causing the affected testicle to shrink.
- Why it happens: The impaired circulation deprives the testicular cells of oxygen and nutrients, leading to cell death and a loss of volume.
- Is it reversible? Unfortunately, once significant atrophy has occurred, it is often not fully reversible. This is why early evaluation, especially in adolescents, is critical. The goal is to preserve testicular size and function before permanent damage sets in.
- Statistic: Studies indicate that up to 50% of adolescents with a varicocele will experience some degree of ipsilateral (same-side) testicular hypertrophy (asymmetry).
3. Chronic Scrotal Pain and Discomfort
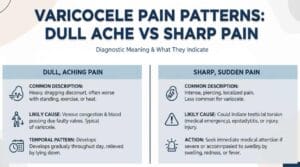
While not all varicoceles cause pain, a significant portion do. This is known as varicocele-related orchalgia.
- The Nature of the Pain: It’s often described as a dull, aching, or heavy sensation that worsens throughout the day, especially with prolonged standing, physical exertion, or during hot weather. The pain typically improves when lying down, as this relieves pressure on the veins.
- Progression: For many, this pain starts as a minor annoyance but can progress to a chronic condition that interferes with daily activities, exercise, and quality of life.
Treatment Options: It’s Not Just Surgery
The good news is that varicoceles are highly treatable. The best approach depends on the severity of your symptoms, your age, and your fertility goals.
Medical Interventions
- Varicocele Embolization: A minimally invasive procedure where an interventional radiologist threads a catheter through a vein to block the faulty vein. Recovery is typically very fast (24-48 hours).
- Surgical Ligation (Varicocelectomy): A urologist makes a small incision to tie off the enlarged veins. Microsurgical techniques are the gold standard, offering high success rates and low complication risks.
Lifestyle and Supportive Management
For men with minimal symptoms who are not currently concerned with fertility, conservative management is an option under a doctor’s guidance.
- Wear Supportive Underwear: This is not a cure, but it is a foundational management strategy. A supportive garment like anatomical scrotal support underwear can lift the testicles, improve blood flow, reduce the feeling of heaviness, and help dissipate heat.
- Avoid Prolonged Standing: Take breaks to sit down if your job requires standing.
- Stay Hydrated and Increase Fiber: Proper hydration and avoiding constipation reduce abdominal pressure, which can aggravate a varicocele.
Case Study: Monitoring vs. Intervention
Patient: “David,” age 28, presented with a palpable left-sided Grade 2 varicocele and mild, intermittent discomfort.
- Year 1 (Monitoring): We opted for conservative management with supportive underwear and annual check-ups. His semen analysis was borderline but acceptable.
- Year 3: David returned, now trying to conceive with his partner for 12 months without success. A repeat semen analysis showed a 40% decline in sperm motility. The dull ache had also become more frequent.
- Decision: David underwent microsurgical varicocelectomy.
- Outcome: Six months post-procedure, his pain had resolved completely. His semen analysis parameters normalized across the board. He reported feeling “lighter” and more comfortable. Within a year, his partner became pregnant.
The Takeaway: David’s case illustrates the progressive nature of varicoceles. What was a minor issue became a significant obstacle to his life goals.
Myth-Busting: Common Misconceptions
Myth 1: “If it doesn’t hurt, it’s fine.”
Reality: Pain is just one indicator. The silent damage to sperm production and testicular size can occur without any discomfort.
Myth 2: “Treatment is only for men trying to have a baby.”
Reality: Treatment is also recommended for adolescents to prevent future infertility and atrophy, and for any man with significant pain that impacts his quality of life.
Myth 3: “Surgery is dangerous and has a long recovery.”
Reality: Modern, minimally invasive techniques are outpatient procedures with very high success rates (>90%) and recovery times measured in days, not weeks.
Conclusion: Your Next Steps
Ignoring a varicocele is a gamble with your reproductive health and comfort. The potential consequences—infertility, testicular shrinkage, and chronic pain—are too significant to dismiss.
The most critical step is to seek a professional evaluation from a urologist. They can accurately grade the varicocele, perform a semen analysis if needed, and assess testicular size. With this information, you can make a collaborative, evidence-based decision about whether treatment is right for you.
Your health is not a passive event. It’s an active pursuit. Taking charge of a varicocele today can preserve your options and well-being for tomorrow.