As a men’s health specialist with over fifteen years of experience counseling patients with scrotal conditions, I’ve witnessed firsthand the anxiety and uncertainty that accompanies a varicocele diagnosis. One question echoes through my consultation room more than any other: “Can this resolve on its own?” Today, I’ll provide you with the evidence-based truth about varicocele natural history, when intervention becomes necessary, and what the latest 2025 research reveals about optimal management strategies.
Understanding the Varicocele: More Than Just “Varicose Veins”
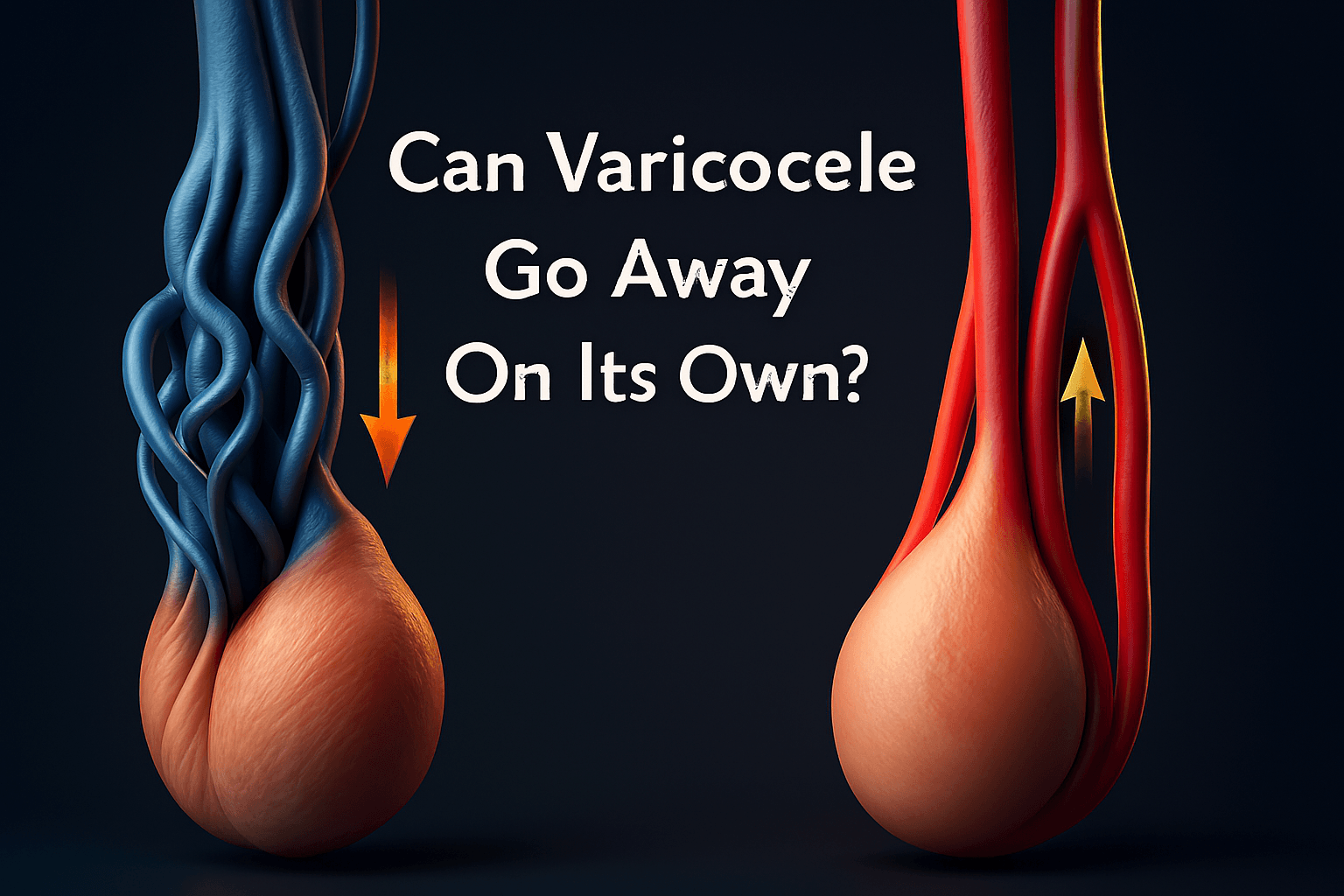
A varicocele represents an abnormal dilation of the pampiniform venous plexus—the network of veins that drains blood from the testicles. Think of it as varicose veins, but in the scrotum rather than the legs.
The prevalence of this condition is significant: it affects approximately 15-20% of all adult males and jumps to 35-40% of men evaluated for infertility. The overwhelming majority (80-90%) occur on the left side, though bilateral cases do occur .
Why this left-sided preference? Anatomy provides the explanation. The left testicular vein drains into the left renal vein at a right angle, creating inherently higher venous pressure compared to the right side, where the testicular vein drains directly into the low-pressure inferior vena cava .
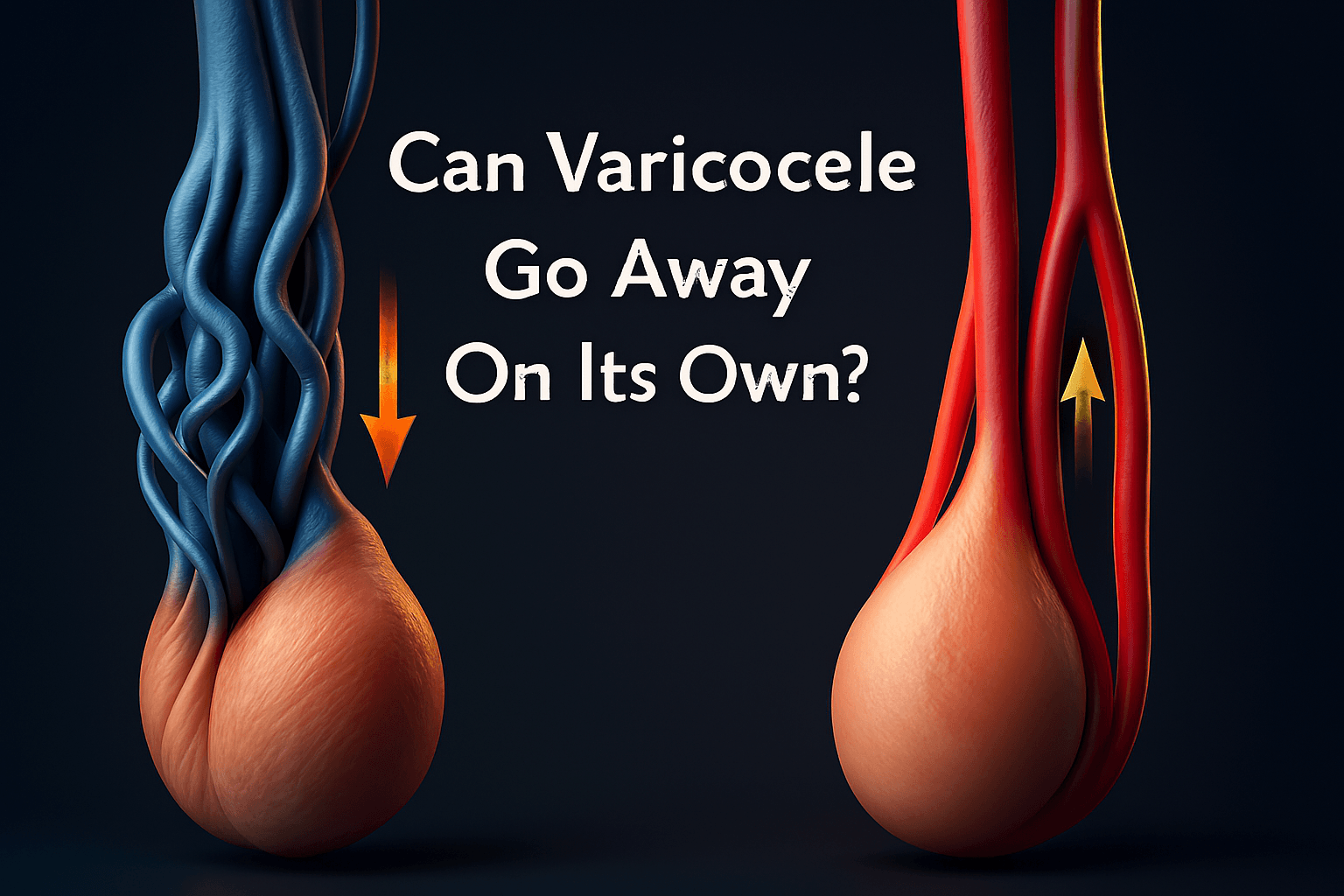
The Central Question: Can Varicocele Resolve Spontaneously?
The short, evidence-based answer is: No, varicoceles do not typically resolve on their own in adult men.
Unlike some temporary physiological conditions that may improve with time or lifestyle changes, a developed varicocele represents a permanent anatomical alteration in the venous system surrounding the testicle. The damaged venous valves cannot regenerate, and the dilated veins will not return to their normal diameter without intervention.
The Anatomical Reason Why Varicoceles Persist
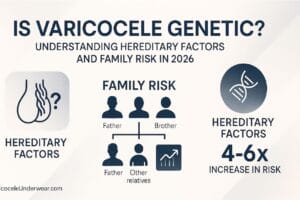
Varicoceles develop due to venous valve failure within the testicular veins. These one-way valves normally prevent blood from flowing backward toward the testicles. When they become incompetent—whether due to genetic predisposition, anatomical constraints, or increased venous pressure—blood begins to pool in the pampiniform plexus .
This valve failure creates a one-way path toward progression. With continued hydrostatic pressure from daily activities like standing, lifting, and straining, the venous dilation typically worsens gradually over time rather than improving.
Clinical evidence from long-term observational studies demonstrates that untreated varicoceles generally remain stable or progress in size—they don’t regress. In my practice, I’ve monitored some patients with mild varicoceles for over a decade without observing spontaneous resolution in a single case.
The Adolescent Exception: A Special Case
The exception to this rule exists in the adolescent population. During puberty, rapid growth and development can sometimes create temporary imbalances between venous pressure and structural support. In some adolescents with grade 1 (minimal) varicoceles, the condition may stabilize or become less apparent as their anatomy matures.
However, even in adolescents, complete spontaneous resolution remains uncommon. The 2025 clinical review in the Journal of Clinical Medicine notes that “progressive testicular atrophy or significant semen parameter abnormalities in adolescents warrant intervention, as spontaneous improvement cannot be relied upon” .
When Natural History Demands Intervention: Consequences of Untreated Varicocele
The decision to intervene with a varicocele depends largely on its clinical consequences. While not all varicoceles require treatment, certain scenarios demand active management.
The Infertility Connection
The most well-documented impact of varicoceles is on male fertility. Multiple pathophysiological mechanisms explain this connection:
Increased scrotal temperature: The pooled blood raises intrascrotal temperature, impairing spermatogenesis
Oxidative stress: Blood stasis generates reactive oxygen species that damage sperm membranes and DNA
Hypoxia: Reduced blood flow limits oxygen delivery to testicular tissue
Toxic metabolite accumulation: Adrenal and renal metabolites may reflux into the testicular circulation
The evidence supporting varicocele repair for infertility is compelling. A 2025 meta-analysis by the Global Andrology Forum found that varicocele repair significantly improved:
Sperm concentration (Standardized Mean Difference: 1.59)
Progressive sperm motility (SMD: 1.85)
Sperm morphology (SMD: 1.07)
Perhaps more importantly, pregnancy rates increase following repair. The same analysis reported significantly higher odds of pregnancy (OR: 1.29) after varicocelectomy .
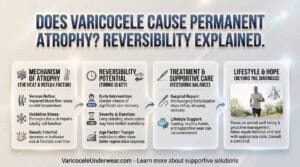
Testicular Atrophy and Hypogonadism
Progressive testicular volume loss represents another clear indication for intervention. The compromised venous drainage and increased temperature can gradually damage the testicular parenchyma, leading to irreversible loss of spermatogenic tissue if left unaddressed.
Additionally, emerging evidence demonstrates that varicoceles can impair testosterone production. Leydig cells, responsible for testosterone synthesis, are particularly vulnerable to the hostile environment created by varicoceles. A 2025 review notes that “varicocelectomy improves serum testosterone level in >80% of patients, with a mean increase between 100 ng/mL and 140 ng/mL” .
Symptomatic Varicoceles: When Comfort Is Compromised
While most varicoceles are asymptomatic, approximately 2-10% of patients experience discomfort . This typically presents as:
A dull, aching pain that worsens with standing or physical exertion
A feeling of heaviness or dragging sensation in the scrotum
Discomfort that improves when lying down
When these symptoms impact quality of life and other potential causes have been excluded, intervention may provide relief.
Modern Treatment Approaches: From Microsurgery to Embolization
For those requiring intervention, contemporary medicine offers several effective approaches.
The Gold Standard: Microsurgical Varicocelectomy
Microsurgical subinguinal varicocelectomy remains the procedure of choice for most specialists, with success rates exceeding 90% and complication rates below 2% . Using an operating microscope, the surgeon meticulously ligates the affected veins while preserving arteries, lymphatics, and nerves. This selective approach maximizes therapeutic benefit while minimizing risks.
Interventional Radiology: Percutaneous Embolization
For appropriate candidates, percutaneous embolization offers a minimally invasive alternative. Under imaging guidance, an interventional radiologist threads a catheter through the venous system to the affected testicular veins, deploying coils, plugs, or sclerosants to block the problematic vessels .
This approach offers comparable success rates to microsurgery with potentially faster recovery, though long-term recurrence rates may be slightly higher.
Non-Surgical Management: The Conservative Approach
For patients with minimal symptoms, normal semen parameters, and no testicular atrophy, observation with periodic monitoring represents a valid strategy. This may include:
Annual semen analysis for fertility concerns
Periodic testicular volume measurement
Symptom monitoring
Additionally, some evidence suggests that lifestyle modifications may help mitigate symptoms, though they won’t reverse the underlying anatomy:
Avoiding prolonged standing
Wearing supportive underwear
Maintaining healthy bowel habits to reduce straining
The table below summarizes the key differences between the main treatment approaches:
| Treatment Approach | Mechanism of Action | Success Rates | Advantages | Considerations |
|---|---|---|---|---|
| Microsurgical Varicocelectomy | Surgical ligation of veins under microscopic guidance | 90-95% | Gold standard, low recurrence, preserves arterial flow | Requires specialized expertise |
| Percutaneous Embolization | Endovascular blocking of veins using coils/sclerosants | 85-90% | Minimally invasive, rapid recovery | Slightly higher recurrence, radiation exposure |
| Observation | Periodic monitoring without intervention | N/A | Avoids procedure risks | Does not address underlying pathology |
Clinical Evidence: What the Latest Research Reveals
Recent high-quality studies have strengthened our understanding of varicocele treatment outcomes:
A 2025 prospective controlled study examined the impact of varicocelectomy on sperm DNA fragmentation—a key marker of sperm health. Researchers found that “the difference in Sperm DNA Fragmentation (SDF) values in the intervention group before and after varicocele repair was 25%” alongside significantly improved pregnancy rates .
Another 2024 meta-analysis confirmed that varicocele repair significantly increases spontaneous pregnancy rates (OR: 1.82) while improving all key semen parameters.
Perhaps most compellingly, a randomized controlled trial focused on couples with recurrent pregnancy loss found that varicocele repair reduced the miscarriage rate from 69.2% to 13.3% while improving pregnancy rates from 19.1% to 44.1%.
Making Your Decision: Expert Guidance
When confronting a varicocele diagnosis, I advise patients to consider these key questions:
What is your reproductive timeline? For men with abnormal semen parameters actively trying to conceive, repair often offers the best chance of natural conception.
Are you experiencing symptoms? Pain or discomfort that affects daily activities warrants stronger consideration for intervention.
Has testicular volume diminished? Documented atrophy suggests progressive damage that likely requires treatment.
What are your testosterone levels? For men with borderline or low testosterone, repair may offer endocrine benefits.
Ultimately, the decision should be made through shared decision-making with a men’s health specialist who can review your individual circumstances, diagnostic findings, and personal goals.
The Bottom Line: Hope Through Science, Not Hope Alone
While the anatomical reality is clear—varicoceles do not resolve spontaneously in adult men—the therapeutic outlook has never been brighter. Modern treatment approaches offer safe, effective solutions for those experiencing symptoms, fertility challenges, or progressive testicular dysfunction.
Rather than hoping for spontaneous resolution that will not come, I encourage patients to pursue evidence-based evaluation and management. With current techniques, we can effectively address the functional consequences of varicoceles while minimizing treatment burden.
For a comprehensive look at all aspects of this condition, I invite you to read our detailed resource: Varicocele: A Comprehensive 2025 Guide to Causes, Symptoms, Diagnosis, and Treatment.
Frequently Asked Questions (FAQs)
Can varicocele disappear naturally with lifestyle changes?
No, lifestyle changes cannot reverse the underlying venous anatomy of a varicocele. While healthy habits may alleviate some symptoms, the damaged venous valves and dilated veins will not resolve without medical intervention. The anatomical changes are permanent once established .
At what age should a varicocele be treated?
Treatment timing depends on symptoms and findings rather than age alone. Adolescents require intervention if showing progressive testicular atrophy. Adults benefit from repair when experiencing infertility, pain, atrophy, or hormonal deficiency. Asymptomatic men with normal testicular function may only need monitoring .
What happens if I never treat my varicocele?
Many men with untreated varicoceles maintain normal fertility and never experience symptoms. However, potential risks include progressive testicular atrophy, declining semen parameters, reduced testosterone production, and in some cases, persistent discomfort. Regular monitoring helps detect any negative progression .
How effective is varicocele surgery for improving fertility?
Modern microsurgical varicocelectomy significantly improves semen parameters in 60-80% of men, with spontaneous pregnancy rates increasing from approximately 17% without treatment to 35-42% after repair. Success depends on individual factors like female partner fertility and varicocele grade .
Can a varicocele come back after treatment?
Yes, recurrence occurs in approximately 5-15% of cases depending on the technique used. Microsurgical approaches have the lowest recurrence rates (1-2%), while embolization and laparoscopic techniques show slightly higher recurrence. Reoperation success rates remain high .
Are there any new treatments for varicocele on the horizon?
Emerging approaches include refined embolization techniques with newer agents, robotic-assisted varicocelectomy, and research into genetic markers that might predict treatment response. Shear wave elastography represents an advance in preoperative assessment and outcome prediction .